Share On Social!
This is part of the “Advancing the Science of Cancer in Latinos: 2022 Conference Proceedings,” which summarizes findings and discussions of the 2022 Advancing the Science of Cancer in Latinos Conference on Feb. 23-25, 2022, in San Antonio, Texas.
Leading Pathways: The Hispanic/Latino Survivorship Study
Dr. Frank Penedo is Associate Director of Cancer Survivorship & Behavioral Translational Sciences at the Sylvester Comprehensive Cancer Center at the University of Miami.
The Leading Pathways Study

Dr. Penedo began by presenting a summary of Leading Pathways, a Hispanic/Latino survivorship study, a collaboration between the Mays Cancer Center at UT Health San Antonio and the Sylvester Comprehensive Cancer Center at the University of Miami. The study has five key aims, the first of which is to establish a Hispanic/Latino survivorship cohort. The study also aims to examine multiple determinants of symptom burden, health-related quality of life (HRQoL), and disease activity. The final three aims include evaluation of psychosocial mediators, evaluation of biological mechanisms, and exploration of potential moderators.
The six-year UG3/UH3 study set out to enroll 3,000 participants, with 50% being Mexican American and 50% from other Latino backgrounds, including approximately 23% from Central and South America and 18% from Cuba. Furthermore, the design calls for 70% of participants to come from a cancer center and 30% from state registries. All of these goals reflect the population in areas surrounding participating cancer centers in Florida and Texas.
Primary Outcomes, Drivers of Outcomes, and Mediators
The primary outcomes of the study are symptom burden (pain, fatigue, sleep, and depression), HRQoL (both general and cancer-specific), and disease activity (cancer remission or recurrence, secondary cancer, incident comorbidity, and palliative or hospice care). In order to fully understand these outcomes, however, drivers of outcomes will also be assessed. These drivers of outcomes are divided into two domains: the non-medical drivers of health domain, and the stress and adversity domain. Another domain includes factors such as income, occupation, education, and access to healthcare, as well as factors like nativity, years in the US, and language preference. The stress and adversity domain covers chronic stress, neighborhood stress, and more.
Another goal of the study is to understand what mechanisms might mediate the association between the drivers of outcomes and the primary outcomes themselves. These mechanisms are divided into a lifestyle and behavior domain, including diet, physical activity, substance use, and treatment adherence; a psychosocial domain covering optimism, spirituality, local integration, and family cohesion; and a biological domain comprised of leukocyte gene expression, cardiometabolic markers, and genetic admixture.
Recruitment to Meet Benchmarks
At the time of presentation, the study was in the third quarter of the first year of UG3. The benchmark for UG3, which covers the first two years of the study, has two key components. The first component is recruitment of 18% of the cohort (~560) in approximately similar distribution to the final cohort with regards to origin, urban/rural, and cancer site. The second benchmark component is collection of baseline questionnaires and blood specimens from 85% of enrolled patients.
Advertisements for the study are disseminated through health system clinics, websites, social media, TV and radio spots, and community events. Other patients are identified through the two state registries, Florida Cancer Data System (FCDS) and Texas Cancer Registry (TCR) Procedures. Participation criteria stipulate that they must be age 18 or older, have completed primary cancer treatment, have no metastatic disease, and have one of the following eight primary cancer diagnoses as confirmed by electronic medical record (EMR) or cancer registry: breast, prostate, colon, kidney, liver, lung, stomach, or uterine.
The assessment schedule for each participant includes seven data collection points: baseline, 6-months, 12-months, and annual follow-ups thereafter. Biosample collection takes place at baseline and at the 12-, 36-, and 60-month follow-ups. The Sylvester Center in Florida and the Mays center in Texas are responsible for biosample collection, processing, and storage, while all gene expression is performed at the University of California, Los Angeles (UCLA).
Potential Impacts of the Leading Pathways Study
Dr. Penedo concluded by outlining the potential impacts of the Leading Pathways study. First, findings will provide novel, critically needed information to inform and guide secondary and tertiary prevention by characterizing actors that influence trajectories and outcomes. Second, the study will discern the differential impact of outcome drivers in Hispanic/Latino populations. Finally, results will identify modifiable psychosocial, behavioral, and biological mechanisms that could be addressed via psychosocial interventions or clinical management to improve survivorship outcomes.
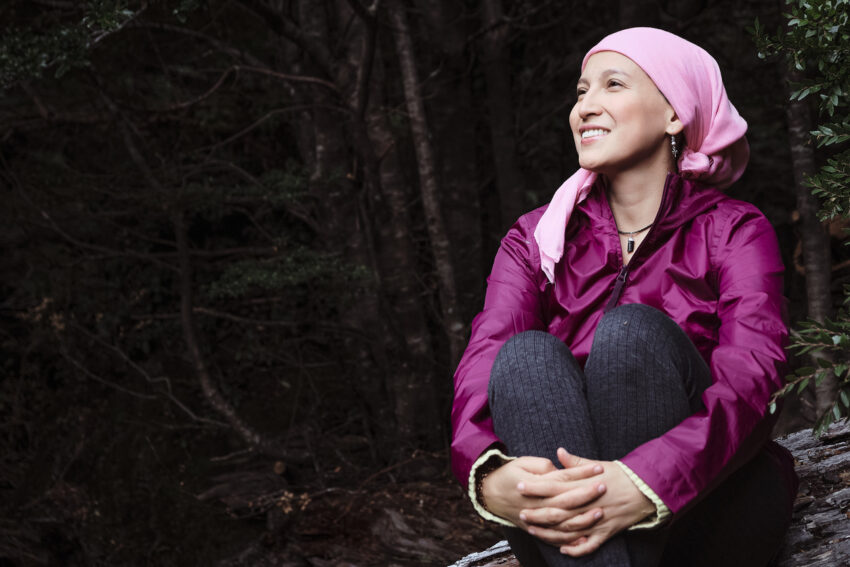
Cancer Care: Loriana’s Story
Loriana Hernandez-Aldama is an Emmy award winning journalist with over 20 years of experience at CNN, FOX, and NBC affiliates in Atlanta, Ga, and Dallas/Ft. Worth and Austin, TX. She is also founder and spokesperson for the ArmorUp for Life campaign.

Loriana is a survivor of acute myeloid leukemia in 2014 and breast cancer in 2020. In the first instance, she endured five rounds of chemotherapy and radiation, overcoming a 30% chance of survival. As a two-time cancer survivor, Loriana emphasizes the mental, physical, and financial brokenness that results from fighting cancer. Depression, anxiety, neuropathy, bone pain, vision issues, and more are issues that are not often discussed in conversations surrounding cancer survivorship.
In response to this gap in awareness, Loriana started the ArmorUp for Life campaign, an initiative that emphasizes not only prevention, but preparation and prehabilitation as well. She explains the importance of ensuring no toxic chemicals are in the home, creating a space for positive energy, and exercising the body, mind, and soul. Loriana also stresses living in the moment and learning to be present; appreciating those who love and support you; and exercising compassion and being empathetic. Finally, the three “P’s” are at the heart of Loriana’s message: you must Prepare yourself for illness, so you can Present well to your medical team, and position yourself to ultimately Prevail.
Read more about Loriana Hernandez-Aldama in a Salud Hero story from the Salud America! program: https://salud-america.org/loriana-hernandez-aldama-warrior-beats-cancer-saves-lives-through-education.
Cancer Care: Daniel’s Story
Daniel G. Garza is an actor, speaks up for HIV and anal cancer, spiritual life coach, and community leader.

As a survivor of anal cancer, Daniel spreads awareness about taboo topics surrounding the illness, including his sex life post-cancer. Chemotherapy and radiation were discussed at length with his physician, but practical changes in his sex life were not even mentioned, like erectile dysfunction, which is a known effect of radiation. Daniel was also had to wear an ostemy bag on his abdomen, which effected him greatly.
These changes and difficulties led to feelings of shame, embarrassment, and unworthiness, says Daniel, which is why therapy is so important for cancer survivors. Both individual therapy, and couples therapy are imperative. Couples tend to create rituals and patterns, especially as they navigate the cancer treatment process, and recapturing the romantic moments in a relationship can be challenging. Finding worth outside of the patient’s body, or their sexual relationship, can help couples regain intimacy after the grueling fight with cancer.
Hear more from Daniel Garza on an episode of the Salud Talks Podcast from the Salud America! program at UT Health San Antonio: https://salud-america.org/men-why-should-you-get-screened-for-cancer-join-this-webinar-6-9-22/
The Therapeutic Alliance and End-of-life Care [Issues] for Latino Cancer Patients
Dr. Ana I. Tergas is Assistant Clinical Professor in the Department of Surgery, Division of Gynecologic Oncology, and the Department of Population Science, at City of Hope Comprehensive Cancer Center.
Understanding the Landscape of End-of-life Care

Dr. Tergas began by defining the goals of palliative care (PC) and end-of-life (EoL) care as outlined by the National Comprehensive Cancer Network (NCCN). The goal of palliative care (PC) is to anticipate, prevent, and reduce suffering and support the best possible quality of life (QoL) for patients, families, and caregivers. End-of-Life (EoL) care becomes the focus when disease-directed, life-prolonging therapies are no longer effective, appropriate, or desired.
EoL Care Challenges for Latino Patients
PC and EoL care are generally underutilized, but disuse can vary by background. Non-White patients tend to be less knowledgeable about EoL care options and use EoL care processes less often, such as advanced care planning (ACP). Because Latino patients are less likely to engage in ACP, they are more likely to receive aggressive EoL care, including increased ICU admissions and chemotherapy use. This aggressive care is associated with poor QoL, minimal survival benefit, and high cost. The likelihood of dying in a hospital is also higher among Latino patients, who receive less prognostic communication, which can lead to inaccurate expectations of survival.
Providing quality EoL care can be challenging in some communities due to population issues, language proficiency, and more. Background often plays a large role, influencing how patients experience and respond to symptoms, make healthcare decisions, and even express distress related to the dying process. Decisions about EoL care can be greatly influenced by differences such as personalismo, a respect for personal relationships; familismo, an emphasis on family loyalty and cohesion; machismo, a view of male dominance and strength; and others.
Certain health care beliefs are held more strongly among some patients. For example, compared to White patients, terminally ill Latino patients are more likely to believe that they are curable, that cancer pain cannot be controlled, that God will perform a miracle to cure them, and that do-not-resuscitate (DNR) orders conflict with their religious beliefs.
The Therapeutic Alliance EoL Care
One aspect of patient care that may improve these EoL care differences is the therapeutic alliance (TA), a construct that encompasses the interrelated and essential dimensions of the patient-physician relationship: trust, respect, understanding, and concern. The TA was first described in psychotherapy literature but has also been successful in cancer patients for improving QoL at EoL, decreasing ICU care at EoL, increasing emotional acceptance of terminal illness, and decreasing invasive interventions at EoL.
TA is measured by the Human Connection Scale, which evaluates five key aspects: the extent to which the patient feels that the oncologist listens to and understands the patient’s concerns about the illness; whether the relationship involves mutual caring and respect; whether the patient understands the information being shared by the oncologist; whether the patient trusts the oncologist; and whether the oncologist and patient work well together.
The Therapeutic Alliance and Patients
A recent study by Dr. Tergas showed that US-born Latino patients, US-born non-Latino patients, and non-Latino immigrants had 8 to 12 times higher odds of having a better TA than Latino immigrants, adjusted for patient education, insurance, and geographic region. The adjusted odds ratio of TA levels among US born Latino patients compared to Latino immigrants, for example, was 11.8 (95% CI: 2.1 – 66.5). The main drivers of this difference were that Latino immigrants did not feel that their oncologist cared about them, took the time to listen, or offered hope.
Dr. Tergas ended by outlining future areas of study, including quantitative analysis of patient-level factors. Focus groups with patients and in-depth interviews with oncologists were another area of interest in order to gain a more nuanced understanding of the TA and its relationship to EoL care for advanced cancer patients. The final priority mentioned by Dr. Tergas was behavioral interventions aimed at improving the TA between oncologists and advanced cancer patients.
Explore More:
CancerBy The Numbers
142
Percent
Expected rise in Latino cancer cases in coming years



