
Share On Social!
Rural populations in the United States face unique health disparities because of their distances from health care providers and limited access to resources.
There are nearly 3.2 million Latinos that live in rural areas of the country, and for them to receive assistance, programs needed to be implemented to lessen these locational barriers. Lower life expectancies and higher rates of pain and suffering are reported in rural areas by the National Advisory Committee On Rural Health and Human Services.

“The Committee is deeply concerned about the gaps between rural and urban life expectancy and mortality that has largely gone unnoticed in the larger discussion about health disparities that tend to focus solely on populations and ignore the geographic aspects of this issue.”
Why is there such a disparity?
Due to a shortage of physicians and rural hospitals closing, these communities are less connected to emergency health services and life-changing appointments with specialty care doctors. These “hospital deserts” have higher rates of poverty and low rates of health education and awareness.
One of the most significant contributors to this inequity is the distance between communities. Since these communities are so isolated, there is no public transportation, which can make doctor appointments and healthy food more readily available.
What Can be Done?
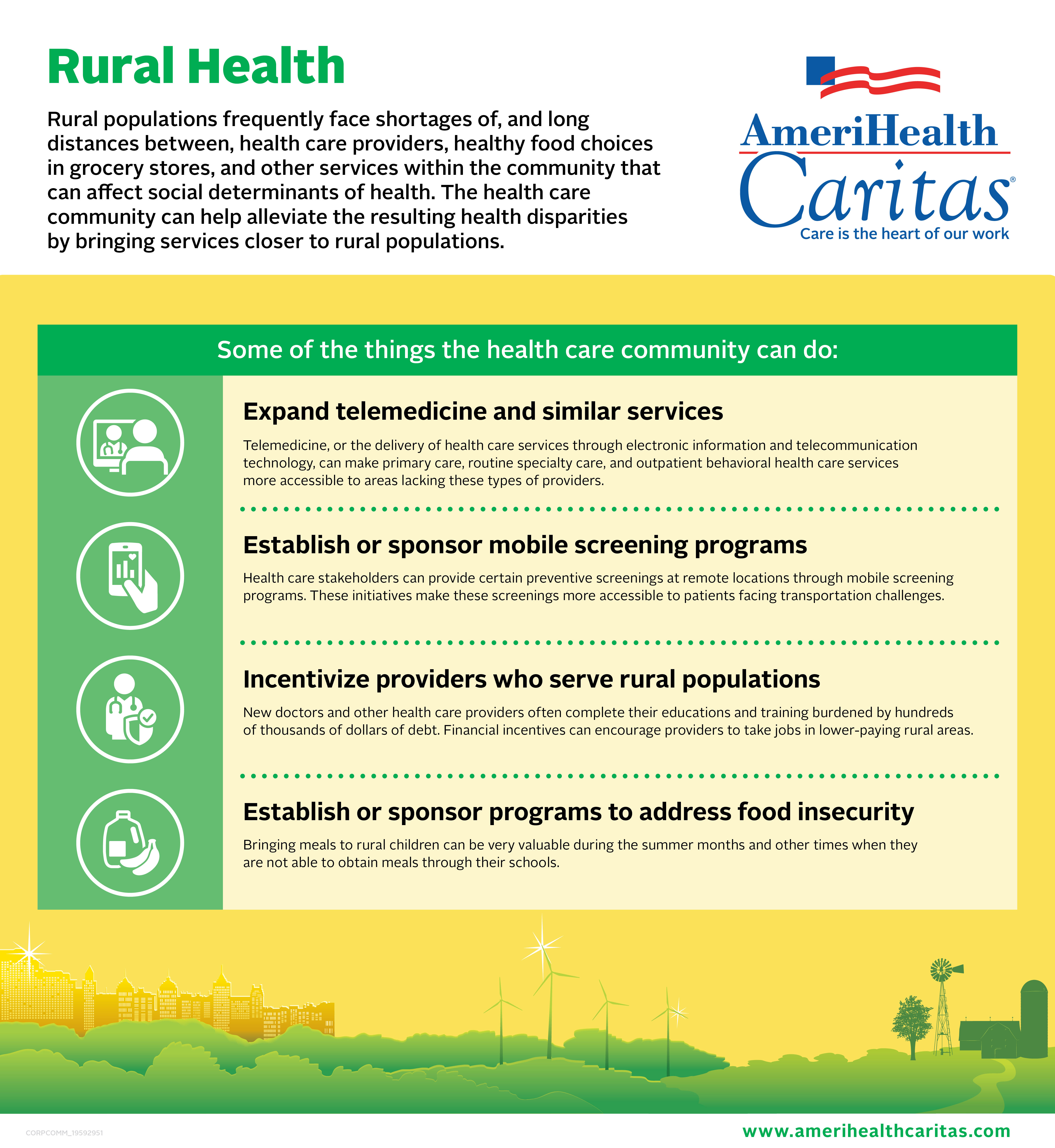 AmeriHealth Caritas, which is a leader in dissolving disparities that are widely overlooked in underserved communities, has collected data about how we can alleviate some of these complications. Moreover, they provided four examples of policy solutions that could help address disparities gaps in rural communities.
AmeriHealth Caritas, which is a leader in dissolving disparities that are widely overlooked in underserved communities, has collected data about how we can alleviate some of these complications. Moreover, they provided four examples of policy solutions that could help address disparities gaps in rural communities.
- New doctors and health care providers should be incentivized to work with rural populations for a period of time with government subsidies to help lessen their thousands of dollars of debt. All while providing high-quality services to those that desperately need it.
- Telemedicine refers to a practice of caring for patients where they are not physically together, but doctors can consult patients directly through video-conferencing tools. This can be appropriate for primary care medicine, where the advice and checkups are more routine.
- Sponsoring mobile screening programs would allow patients with accessibility challenges to efficiently screen for health issues that they may not have studied. The MD Anderson Cancer Center has a mobile mammography van that provides women with early breast cancer detection.
- Establishing a program to address food insecurity in these rural communities is also very important. It can be difficult for families and children to have access to healthy meals. Food insecurity is a massive problem in America. Not knowing where or when you are getting your next meal from is common in these rural populations. Implementing school food pantries and sponsoring community gardens can address these issues while inspiring lifestyle changes.
In addition to these problems, rural populations “are more likely to die from heart disease, cancer, respiratory disease, stroke, and unintentional injuries than their urban counterparts.” Latinos face even higher risks of heart disease and cancer, so it is essential to mobilize these communities to prevent this continuation of inequality of resources.
Explore More:
HealthBy The Numbers
142
Percent
Expected rise in Latino cancer cases in coming years



… [Trackback]
[…] Read More: salud-america.org/dr-francisco-g-cigarroa-the-first-latino-chancellor-of-the-university-of-texas-system/ […]