
Share On Social!
Where we live plays a significant role in our healthcare. But many Americans don’t have easy access to the healthcare they need.
In the United States, 5% of rural hospitals have shut down since 2010 with maternal and obstetric care taking the hardest hit. About 16% of the mainland United States are 30 miles or more away from the nearest hospital, CNN reports.
These areas with no access to a hospital are called “hospital deserts.”
Many regions that are hospital deserts also have higher rates of poverty and income gaps, leaving many residents with no options for emergency or regular healthcare.
“There’s a lot of people out in the rural community who feel like they’ve been forgotten,” Jessica Thompson, a registered nurse who lives in a hospital desert in Tonopah, Nev., told CNN.
Troubling Facts About Healthcare Access
 Hospital deserts are becoming a national crisis, both in urban and rural areas:
Hospital deserts are becoming a national crisis, both in urban and rural areas:
- Approximately 30 million Americans do not live within an hour of a trauma center.
- Due to distances to emergency rooms, accidental deaths are 50% higher in rural areas in comparison to urban areas.
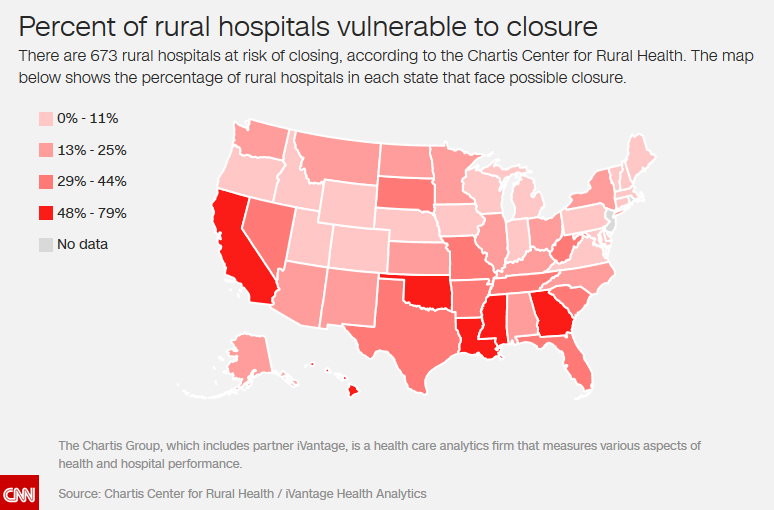
- Nearly 673 rural hospitals are at risk of shutting down.
For patients experiencing a heart attack or stroke, timing is everything.
“Every minute that you can get the patient into treatment sooner will represent some brain cells that are saved,” Dr. Jeremy Brown, director of the National Institute of Health’s Office of Emergency Care Research, told CNN.
What Is Causing Countless of Closures?
The main source of hospital closures is due to financial challenges.
Socioeconomic status significantly contributes to a hospitals financial challenges. Since 2007, rural areas in America have had declining earnings. Furthermore, earnings are 25% lower than suburban and urban areas.
Not being able to adapt technology as well as not being able to attract and keep adequate staff is also problematic.
In 2015, the Save Rural Hospitals Act was introduced by the House of Representative with the hopes of maintaining rural hospitals through financial relief as well as stopping recent healthcare spending cuts that had led to numerous rural hospital closures across America.
However, the bill has yet to be passed.
In the mean time, people are stepping up for rural healthcare.
Rabbit Transit in New York gives rides to rural senior citizens to shop for groceries or reach farmer’s markets. In Suffolk County, N.Y., Minerva Perez She helped create a unique free van ride program that bridges transportation gaps. It also gives her an advocacy platform to improve public transportation at the local level.
In Minnesota, planned public transit improvements will enable more buses across the Twin Cities. This would connect a mostly Latino mobile home community to healthcare and opportunity.
Learn more about rural healthcare!
By The Numbers
25.1
percent
of Latinos remain without health insurance coverage



