Share On Social!
You may be wearing PPE on your face right now.
A mask is a common form of PPE, or “personal protective equipment,” as are respirators, gowns, gloves and eye protection frequently worn by frontline healthcare workers.
These all help protect the wearer – you! – from germs that can make people sick.
But they have a second important function, too.
“So, the unique thing about PPE in healthcare is that it actually serves two purposes, and both of those purposes are really important. One part is to protect you, but the other part is to protect your patient and coworkers from germs that you might be carrying,” said Dr. Abigail Carlson, an infectious diseases physician with the CDC, as part of CDC Project Firstline’s Inside Infection Control video series.
What is PPE and How Does it Work?
For those who do not understand why PPE is so important, Dr. Carlson points out the common use of PPE in many jobs, such as firefighters.
“It’s not just in healthcare that we have this. One great example is a firefighter. They use equipment to protect them from the hazards that their job, a helmet to protect them from things falling down on their head,” Dr. Carlson said. “They might use gloves, boots, and a uniform or a pants and coat to protect them from heat. They might protect themselves from smoke with a mask. All of that is personal protective equipment, or PPE.”
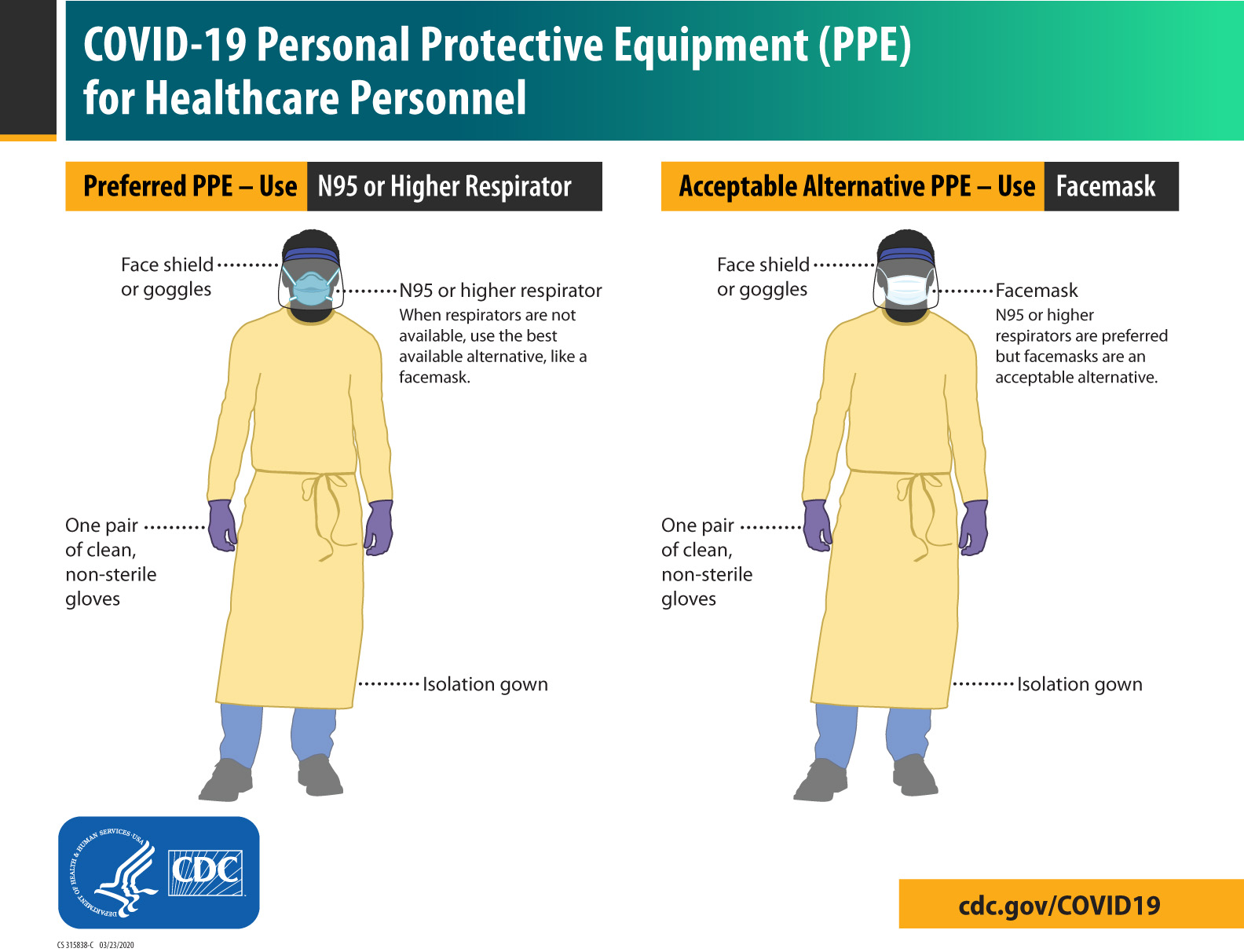 In healthcare, PPE is used to protect the wearer from dirty surfaces or equipment, prevent exposure to germs from patients, and to keep the wearer from spreading germs to patients, visitors, coworkers, and the environment.
In healthcare, PPE is used to protect the wearer from dirty surfaces or equipment, prevent exposure to germs from patients, and to keep the wearer from spreading germs to patients, visitors, coworkers, and the environment.
Dr. Carlson notes three examples of PPE in healthcare settings:
- Wearing a mask: You’re protecting your nose and mouth from splashes and sprays of infected fluids that could make you sick, and you’re also keeping a lot of germs that you are breathing out from reaching other people or the environment.
- Using a respirator: You’re protecting your nose and mouth from splashes and sprays, plus filtering out things you could breathe in that could make you sick.
- Wearing gowns and gloves: They keep germs off of your hands and clothes; by taking off gowns and gloves when you’re supposed to, you also keep germs that have gotten on you from spreading to other people, or the things around you.
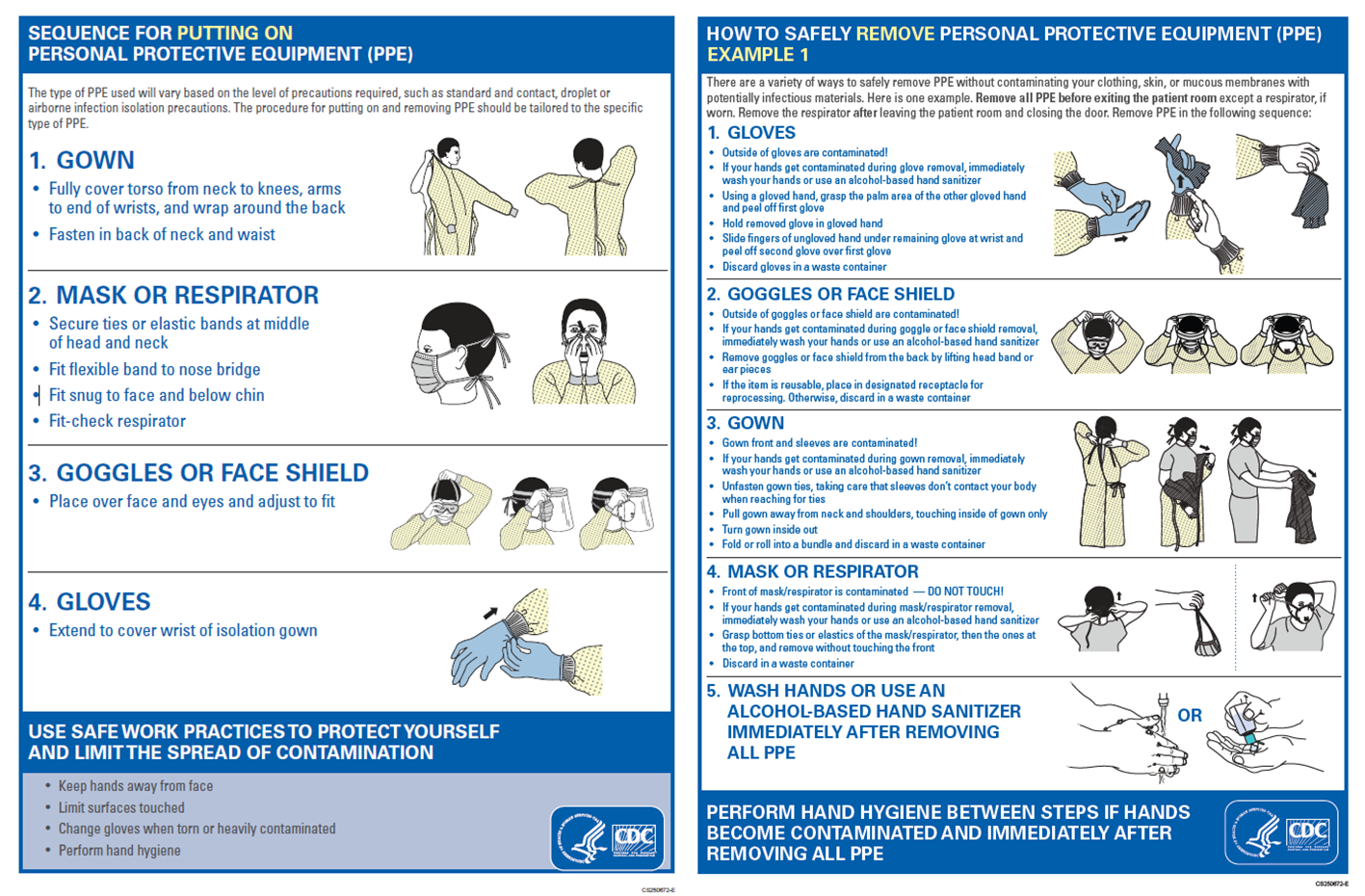 When used correctly, PPE can reduce the spread of germs.
When used correctly, PPE can reduce the spread of germs.
“We like to say PPE doesn’t have a brain. It doesn’t have a mind of its own,” Dr. Carlson said. “It relies on you, your brain, your mind, to think about how to use it and use it correctly. So, think through using your gear, what you’re using, how you’re using it, is it the right time, and you have to go through that process every time to just be sure that you’re protected, you’re protecting your patient, as you’re about to go do your work.”
What is Project Firstline?
Still, Dr. Carlson notes, there are still other ways to implement infection control in healthcare settings.
These include:
- Screening, triage, and patient placement
- Maintaining patient care equipment and environmental surfaces (including cleaning and disinfection)
- Staying home when you’re sick
- Keeping up with recommended vaccinations
“Even though [PPE is] really important, we have to remember, it’s not magic,” she said. “It’s not the only thing you do. In fact, it’s one of many tools that we use protect you in your daily work to avoid being exposed to germs. So, we use other things like barriers, telemedicine, improving ventilation, good cleaning, and good disinfection practices, but when those things aren’t going to be enough, and you have to interact with your patient to provide good care, and there is risk of spreading germs, you want PPE to reduce that risk both for you and your patient, so that it doesn’t spread between the two of you.”
Healthcare workers can access more information about infection prevention and control in healthcare by visiting resources from Project Firstline.
Project Firstline creates resources, including videos and shareable images, web buttons, posters, and print materials. They also have facilitator toolkits to help workers lead trainings even if they are not an infection control expert.
Salud America! at UT Health San Antonio is working with the National Hispanic Medical Association to bring CDC Project Firstline infection control educational content to healthcare workers, so they are equipped with the knowledge they need to protect themselves, their facilities, and their patients (from Latino and all communities) from infectious disease threats in healthcare settings.
You can read these articles:
- What is Project Firstline?
- What’s a Virus?
- How Does Infection Control Work on COVID-19 Variants Like Omicron?
- Contact Time: What is It and How Does it Impact Infection Control?
- The Surprising Difference Between Cleaning and Disinfection
- What’s a Respiratory Droplet and Why Does It Matter?
- Why Do Cleaning and Disinfection Matter in Healthcare?
- We Need to Talk about Hand Hygiene Again
- What is the Goal of Infection Prevention and Control in Healthcare Settings?
- The Intersection of Infection Prevention and Control and Healthcare Equity
“Healthcare teams in hospitals, nursing homes, and other care settings are the front lines against the spread of infection,” said Dr. Amelie G. Ramirez, director of Salud America! at UT Health San Antonio. “CDC’s Project Firstline is bolstering those efforts by developing evidence-based tools that can be delivered in a variety of ways to make infection control learning convenient and accessible for busy healthcare staff.”
LEARN MORE ABOUT PROJECT FIRSTLINE!
Editor’s Note: This article is part of a collaboration between Salud America!, the National Hispanic Medical Association, and the CDC’s Project Firstline. To find resources training materials, and other tools to bolster knowledge and practice of infection control, visit Project Firstline and view Salud America!’s infection control content.
By The Numbers
142
Percent
Expected rise in Latino cancer cases in coming years



