Share On Social!
Viruses are a type of germ that can infect a host body and cause illness, like a cold or COVID-19.
A virus uses living things, like animals and people, to make copies of themselves. Then they keep spreading from one living thing to another.
Viruses can lead to numerous illnesses, including: bronchitis, the flu, the common cold, and COVID-19.
Fortunately, if you know a little bit about viruses, then it’s easier to understand why the things we do for infection control work to stop them from spreading and making people sick.
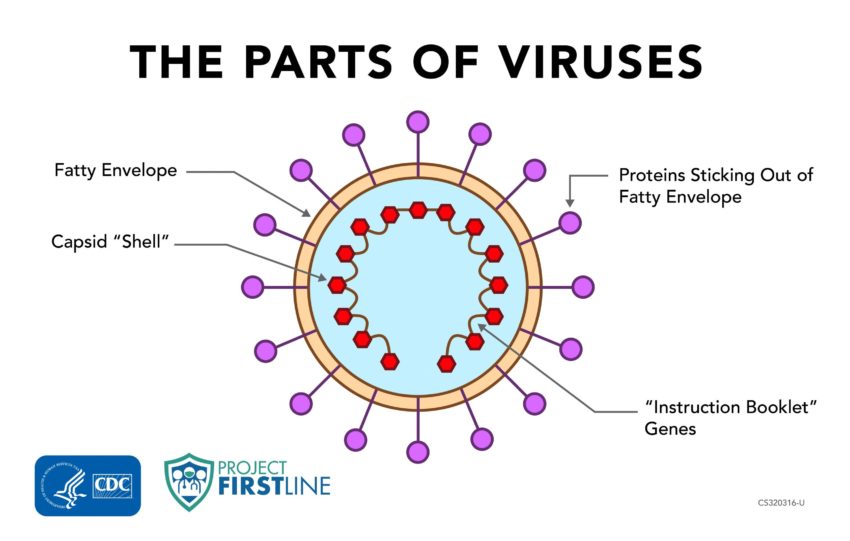
CDC’s Project Firstline, an initiative to inform and train healthcare workers about infection prevention and control, helps us explore the three main parts of viruses:
1. The Genes of Viruses
Genes are the first main part of a virus.
All viruses have genes, just like we have genes. The genes contain all the information needed for the virus to make copies of itself.
You can think of these genes as the “instruction booklet” or the “blueprint” of the virus.
2. The Proteins of Viruses
Viruses also have proteins, just like we have proteins.
Most of the proteins in a virus come together to create a shell, called a “capsid,” that protects the “blueprint” genes from getting damaged.
Some proteins stay inside the shell, and they’re only used when it’s time to build more virus copies.
Other proteins stick out from the shell to help the virus get from one place to another in the body and to help it spread from one person to another.
3. The Envelopes of Viruses
Some viruses have another layer. This layer is called an envelope. Not all viruses have this envelope, but SARS-CoV-2, the virus that causes COVID-19, does.
You can think of this like an envelope that we put letters in to protect them when they are mailed.
The envelope around the virus is made of fats with some proteins mixed in.
The envelope has some proteins sticking out of it, just like the shell does, to help the virus get around and into cells and to help it spread from one person to another.
How Can You Help Stop Viruses from Spreading in Healthcare Settings?
Salud America! at UT Health San Antonio is working with the National Hispanic Medical Association to bring CDC Project Firstline infection control educational content to healthcare workers, so they are equipped with the knowledge they need to protect themselves, their facilities, and their patients (from Latino and all communities) from infectious disease threats in healthcare settings.
 For COVID-19, Project Firstline recommends that healthcare workers use the following infection control actions and tools in healthcare settings:
For COVID-19, Project Firstline recommends that healthcare workers use the following infection control actions and tools in healthcare settings:
- Cleaning hands. Soap and water and alcohol-based hand sanitizer break apart the envelope that holds the virus together.
- Creating good ventilation. Good indoor ventilation is important for clearing air that might have respiratory droplets in it.
- Practicing physical distance. Maintaining physical distance helps people avoid breathing in each other’s respiratory droplets.
- Using appropriate personal protective equipment when caring for suspected or confirmed COVID-19 patients. An N95 respirator protects healthcare workers from breathing in virus that’s in respiratory droplets, and eye protection keeps respiratory droplets from landing in the eyes.
- Using gloves and gowns. These materials prevent healthcare workers from spreading germs to their nose, mouth and eyes through touch, as well as preventing spread into the work environment.
Moreover, healthcare workers can access more information about infection prevention and control in medical settings by visiting resources from Project Firstline.
Project Firstline creates resources, including videos and shareable images, web buttons, posters, and print materials. They also have facilitator toolkits to help workers lead trainings even if they are not an infection control expert.
“I think there’s probably not a single healthcare worker in the country that thinks hand hygiene is bad. But I do think that there are people who may not think about all of the times they need to do that,” Dr. Michael Bell, deputy director of the CDC’s Division of Healthcare Quality Promotion, told Infection Control Today.
“An example is cleaning your hands before putting on non-sterile gloves. A lot of people will react to that and say, ‘Well, I’m putting on gloves. So why do I need to clean my hands? I’ll clean them as soon as I’m done and take my gloves off.’ But the rationale is if you’ve got something on your hands, and you reach into a glove box, a box of clean gloves, and contaminate them, not only are you then contaminating the gloves you’re putting on, but you’re contaminating other gloves that other healthcare workers are going to have to reach in to use. Putting both them at risk, and their patients.”
Editor’s Note: This article is part of a collaboration between Salud America!, the National Hispanic Medical Association, and the CDC’s Project Firstline. To find resources training materials, and other tools to bolster knowledge and practice of infection control, visit Project Firstline and view Salud America!’s infection control content.
Explore More:
Infection ControlBy The Numbers
142
Percent
Expected rise in Latino cancer cases in coming years



[…] The pandemic is another chapter in the bitter story of American racism and inequality. Black and Latinx people are being infected and are dying at much higher rates than white Americans. Many people of […]
[…] coronavirus has killed over 61,000 Latinos in America according to the CDC, accounting for over 18.2% of the total COVID deaths in the […]
[…] Whereas Hispanics make up 11% of D.C.’s inhabitants, they signify 19% of the COVID cases, and 14% of the deaths. Equally, 46% of D.C.’s residents are Black, they usually make up an alarming 75% […]
[…] and historical mistreatment. According to the U.S. Centers for Disease Control and Prevention, Latino and Black American communities are three times more likely to become infected with […]
[…] Covid pandemic has hit the Latino community particularly hard, and data from the nonprofit health equity advocacy group Salud America! shows Latinos lead in the 0-24 age […]
[…] the pandemic, Latinos took major blows, both in terms of COVID-19 cases and also from the economic recession under former President Donald Trump. Nearly half (49%) of […]
[…] the positive trend, the harm may have already been done. The pandemic has disproportionately impacted Latino communities. Reuters reported that election-related or political disinformation that […]
[…] pesar de la tendencia positiva, es posible que el daño ya esté hecho. La pandemia ha impactado desproporcionadamente Comunidades latinas. Reuters informó que la desinformación política o relacionada con las […]
[…] residentes blancos muestran una tasa mucho más baja con 10 muertes por cada 100,000 habitantes(8 9) . Los afroestadounidenses por su parte, denuncian subsistemas de salud que les segregan […]
[…] https://salud-america.org/coronavirus-case-rates-and-death-rates-for-latinos-in-the-united-states/ […]
[…] https://salud-america.org/coronavirus-case-rates-and-death-rates-for-latinos-in-the-united-states/ […]
[…] communities have the second-highest number of COVID-19 cases in the U.S. They’re also more likely to become hospitalized and die from the disease than other […]
[…] total, around 160,000 Latinos were killed by COVID-19. This accounts for 16% of the 1 million deaths in the country. The […]