Share On Social!
This is part of the Salud America! The State of Latino Early Childhood Development: A Research Review »
Growing up feeling safe, secure, and loved is essential for the healthy development of all children.14
Nationally, over 46% of U.S. youth—34 million children under age 18—have had at least one ACE, and more than 20% have had at least two.15
By age 6, 70% of children in a sample of families investigated for adverse childhood experiences (ACEs) have ACEs that may have negative effects on many aspects of their developmental.8,9,16,17
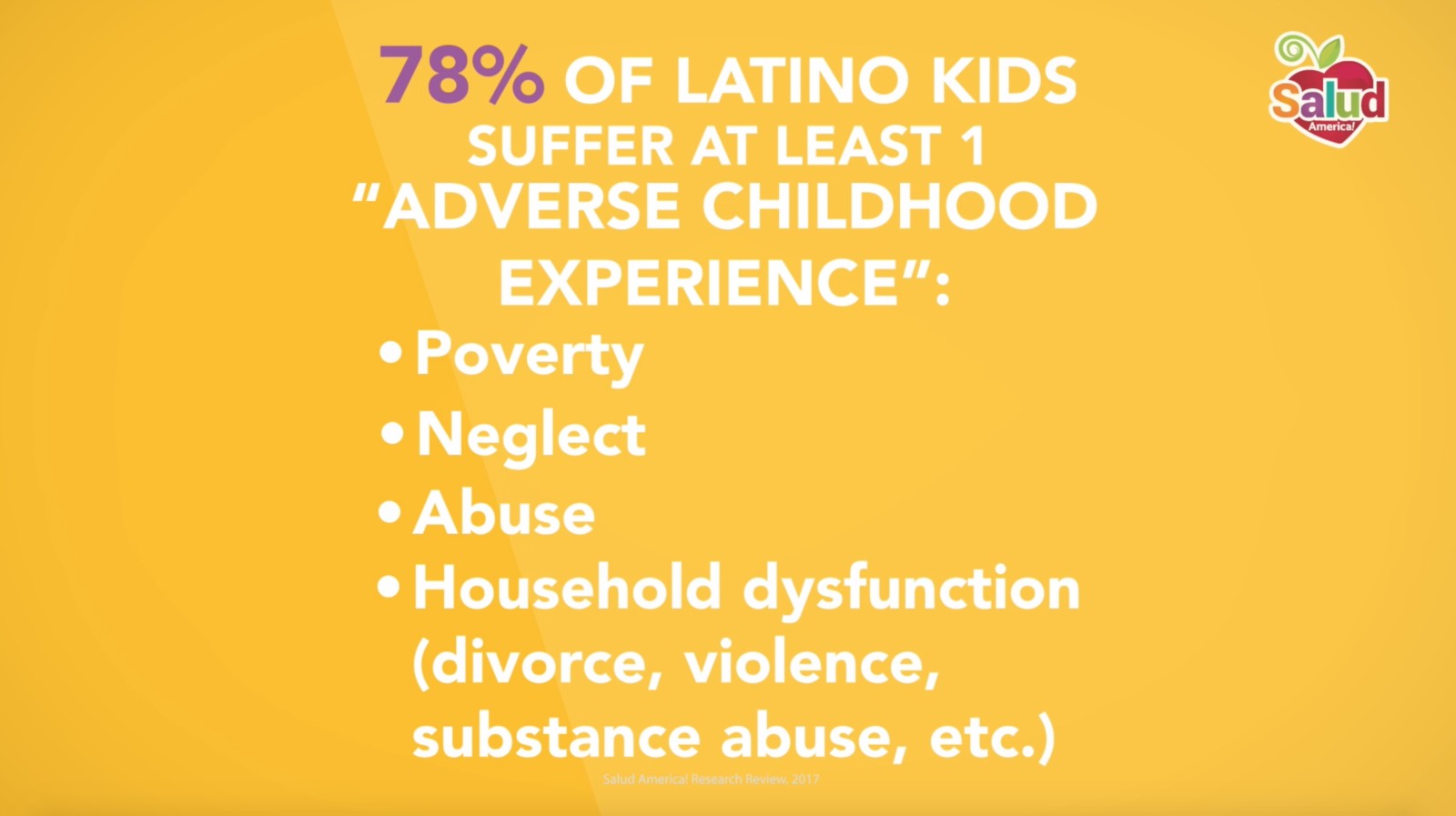
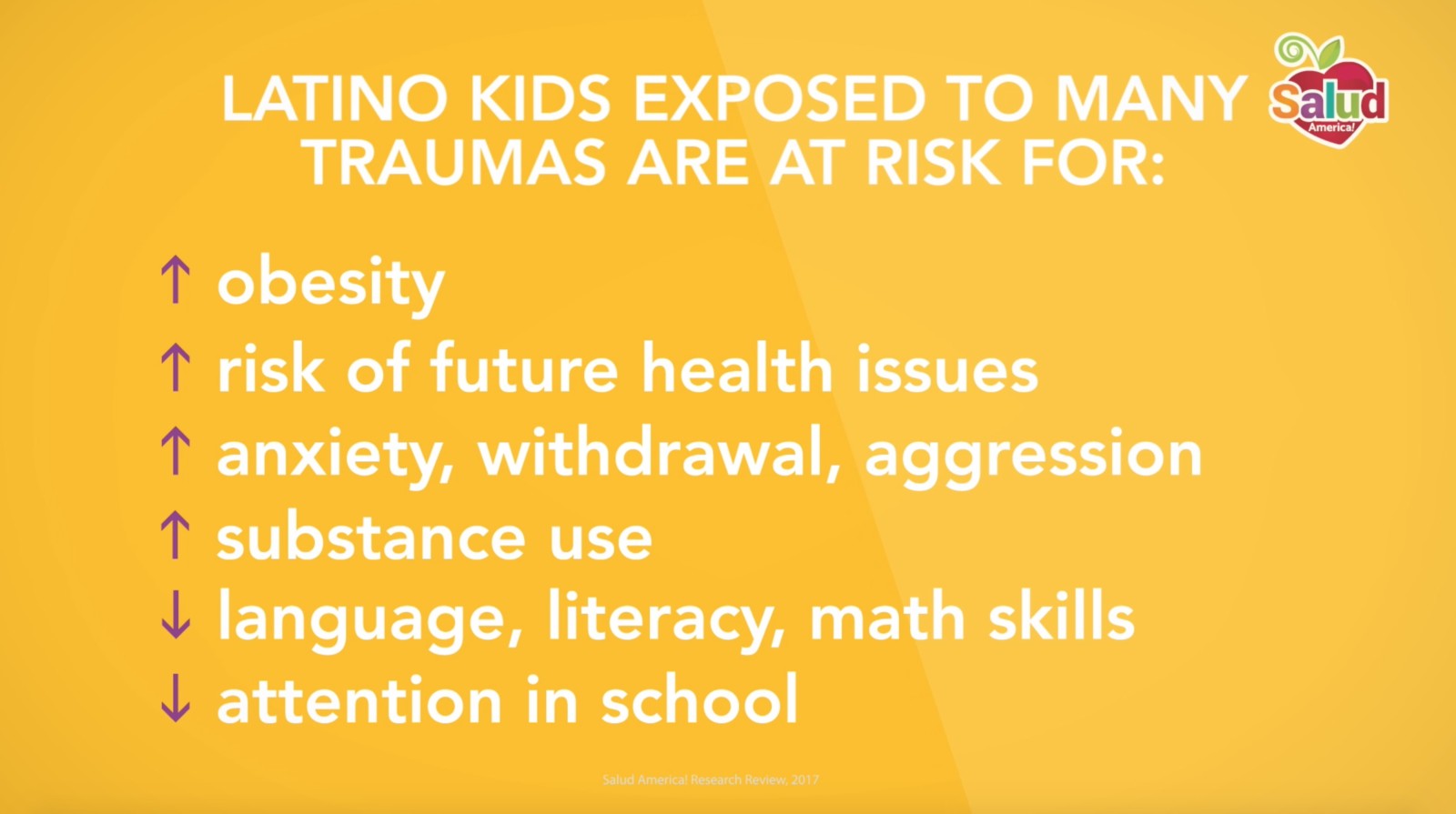
ACEs may include parental domestic violence, substance use disorder, mental illness, criminal justice involvement, child abuse and/or neglect, poverty/homelessness, and parental death, among others.18 Multiple studies have shown that children exposed to ACEs are more likely to develop physical, mental, behavioral, psychosocial, and/or cognitive issues than children who have not been exposed to ACEs, and these effects can extend into adolescence and adulthood.19–26
 About 30 percent of Latino children in U.S.-native families reported two or more ACEs,27 compared to 16 percent of Latino children in immigrant families. Unmeasured confounders may buffer Latino children from exposure to ACEs in immigrant families, and/or negative effects of unmeasured factors for Latino children in U.S.-native families. Also, questions about ACEs may not capture the adverse experiences specific to immigrant families; in fact, it is possible that adverse experiences and environments that are specific to the immigrant experience are not reflected in traditional measures of ACE exposure.
About 30 percent of Latino children in U.S.-native families reported two or more ACEs,27 compared to 16 percent of Latino children in immigrant families. Unmeasured confounders may buffer Latino children from exposure to ACEs in immigrant families, and/or negative effects of unmeasured factors for Latino children in U.S.-native families. Also, questions about ACEs may not capture the adverse experiences specific to immigrant families; in fact, it is possible that adverse experiences and environments that are specific to the immigrant experience are not reflected in traditional measures of ACE exposure.
For both the native and immigrant groups, parental divorce and economic hardship were the most prevalent ACE exposures. Poor maternal mental health and single-woman family structure had the strongest associations with ACE exposure in both groups. Similarly, in both groups, low-income or middle-income households (≤200% of FPL or 201%–400%) were associated with twice the odds of exposure to two or more ACEs compared with those from a high-income reference group.
Many studies have evaluated the multitude of effects of ACEs on Latino children specifically, and these are categorized below by outcome measure.
Physical Health and ACEs
The Hispanic Community Health Study/Study of Latinos (HCHS/SOL) Sociocultural Ancillary Study evaluated ACEs in 5,117 Latino adolescents and adults (ages 18-74) and found that 77.8% experienced at least one ACE, which stands in contrast to the 46% of youth in general who are exposed to ACEs. The same study on Latino adolescents and adults found that 28.7% experienced four ACEs or more.16,28
 Among the ACEs reported, the most common were parental separation/divorce, emotional or physical abuse, and household alcohol/drug abuse. After controlling for demographics and risk factors in this Latino population, ACEs were found to be positively associated with multiple health-related conditions later in life, including alcohol and tobacco use, coronary heart disease, chronic obstructive pulmonary disease, and cancer.
Among the ACEs reported, the most common were parental separation/divorce, emotional or physical abuse, and household alcohol/drug abuse. After controlling for demographics and risk factors in this Latino population, ACEs were found to be positively associated with multiple health-related conditions later in life, including alcohol and tobacco use, coronary heart disease, chronic obstructive pulmonary disease, and cancer.
Although this study did not find an association between ACEs and asthma, another study that used 2011 to 2012 data from the National Survey of Children’s Health (N = 92,472; ages 0-17; 10.3% Latino) reported a 4.46 times increase in lifetime asthma among Latino children experiencing four ACEs compared with those experiencing no ACEs. Importantly, white children experiencing four ACEs had only a 1.19 times increase in lifetime asthma.29
Another study that used data from the HCHS/SOL Sociocultural Ancillary Study found that economic hardship during childhood was associated with shorter height among Latinos regardless of birth place and with greater adiposity in U.S.-born Latinos only.28 Short stature and adiposity may lead to chronic health issues later in life, but this study did not assess for those associations in the adult participants. Further research is needed to understand the full effects of childhood poverty on the development of chronic diseases in Latinos.
The Carolina Abecedarian Project (ABC) was designed as a social experiment to test if stimulating the early care environment from birth to age 5 could prevent the development of mild mental retardation in disadvantaged children.29 Curriculum emphasized development of language, emotional regulation, and cognitive skills, as well as caregiving, supervised play, two meals, one snack, and primary pediatric care for the first five years of life. In their mid-30s, participants had lower blood pressure, better lipid levels, and lower abdominal obesity. They were less likely to have Metabolic Syndrome and had lower risk of experience Coronary Heart Disease. Of participants and non-participants studied, those who are obese or severely obese in their mid-30s are already on a trajectory of above-normal BMI in the first five years of their lives.
Children randomly assigned to stimulating early care from birth to age 5 had significantly lower risk factors for cardiovascular and metabolic diseases in their mid-30s.31
Mental Health and ACEs
A study of data on youth from the Florida Department of Juvenile Justice (N = 64,329; 15.37% Latino) evaluated the effects of ACEs on suicide attempts, as mediated by maladaptive behavior including personality development (aggression and impulsivity) and problem behaviors (school difficulties and substance use disorder).32
Latino youth with higher ACE scores were found to have significantly and directly increased odds of attempting suicide, as well as school misconduct. Although Latino youth were less likely to experience ACEs and attempt suicide than their white counterparts, they were more likely to have aggression, which was a predictor of suicide. Efforts should be made to identify ACEs and developmental/behavioral issues early to prevent potential suicidal behavior in Latinos and all children.
Childhood maltreatment exposure was associated with mental health problems classified as internalizing (anxiety, depression, withdrawal, somatic complaints) and externalizing (delinquency, aggression) among Latino, non-Latino white, and black groups in one study of the use of mental health services by children who had been exposed to some form of maltreatment and were being investigated by child welfare services.33
The study (N = 1,600; 19.3% Latino) found that neither internalizing nor externalizing problems predicted the use of mental health service in Latinos, which is contrary to previous findings suggesting that Latinos with externalizing problems are just as likely to use mental health services as their white and black counterparts.34 The lack of significant association is potentially attributed to the smaller Latino sample size in this study, as noted by the authors. However, other factors such as cultural and family issues may dissuade Latino parents from following through on referrals made to mental health services after their child’s exposure to maltreatment.
Thus, additional research is needed to identify the predictors of mental health service use among Latino youth and develop the necessary assessment and counseling tools to identify at-risk Latino youth and get them the mental health services they need to improve their mental health.
Read the full Salud America! research review on mental health and Latino children.35
Substance Use Disorder and ACEs
A study of 1,259 Puerto Rican youth (10 or older at baseline) from the South Bronx, New York and San Juan, Puerto Rico found that child maltreatment, parental maladjustment, and sociocultural stressors increased the risk of early alcohol use (by age 14) in this youth population.36 Linear relationships were observed between the number of ACEs to which a child was exposed and the risk of early drinking.
Another study of 1,420 Latino emerging adults in Southern California found that the presence of ACEs was significantly associated with substance use or substance use disorder, specifically cigarette, alcohol, marijuana, and hard drug use. As the number of ACEs increased, so did the substance use for all substances.37 Depressive symptoms stemming from ACEs can also increase the risk of substance use/abuse, so identifying and treating depression may help to reduce the substance use/substance use disorder, although it is likely that many factors are involved and further symptoms assessment and intervention may be warranted.38
Education, Achievement and ACEs
Children ages 3 to 5 who have had two or more ACEs are over four times more likely to have trouble calming themselves down, be easily distracted, and have a hard time making and keeping friends.
More than three of four children ages 3-5 who have been expelled from preschool also had ACEs.39
A study of urban children (N = 1,007; 24% Latino) used data from the Fragile Families and Child Wellbeing Study, a national urban birth cohort, to evaluate the effects of ACEs on kindergarten outcomes.22
Children exposed to three or more ACEs were more likely to have below-average language and literacy skills, poor math and emergent literacy skills, attention problems, and aggression in kindergarten. However, the data were not analyzed separately for Latinos.
More from our The State of Latino Early Childhood Development: A Research Review »
- Introduction & Methods
- Key Research Finding: Latino Childhood Trauma
- Key Research Finding: Healthy Lifestyles
- Key Research Finding: Early Care and Education
- Key Research Finding: Strategy—Improve Early Care
- Key Research Finding: Strategy—Boost School Readiness
- Key Research Finding: Strategy—Reduce Childhood Trauma
- Key Research Finding: Strategy—Incorporate Family Values
- Key Research Finding: Strategy—Support Moms
- Policy Implications
- Future Research Needs
References for this section »
8. Braveman, P., Egerter, S., Arena, K. & Aslam, R. Early Childhood Experiences Shape Health and Well-Being Throughout Life. (Robert Wood Johnson Foundation, 2014).
9. Bright, M., Knapp, C., Hinojosa, M., Alford, S. & Bonner, B. The Comorbidity of Physical, Mental, and Developmental Conditions Associated with Childhood Adversity: A Population Based Study. Matern. Child Health J. 20, 843–853 (2016).
14. Newton, J. Prevention of mental illness must start in childhood: growing up feeling safe and protected from harm. Br J Gen Pr. 65, e209–e210 (2015).
15. Bethell, CD, Davis, MB, Gombojav, N, Stumbo, S, Powers, K. Issue Brief: A national and across state profile on adverse childhood experiences among children and possibilities to heal and thrive. Johns Hopkins Bloomberg School of Public Health, October 2017. http://www.cahmi.org/wp-content/uploads/2017/10/aces_brief_final.pdf
16. Clarkson Freeman PA, Prevalence and Relationship Between Adverse Childhood Experiences and Child Behavior Among Young Children. Infant Mental Health Journal [serial online]. November 2014;35(6):544-554. Available from: Psychology and Behavioral Sciences Collection, Ipswich, MA. Accessed March 16, 2018.
17. Robert Wood Johnson Foundation. Early Childhood Experiences Shape Health and Well-Being Throughout Life. (2014).
18. Lucenko, B. A., Sharkova, I. V., Huber, A., Jemelka, R. & Mancuso, D. Childhood adversity and behavioral health outcomes for youth: An investigation using state administrative data. Child Abuse Negl. 47, 48–58 (2015).
19. Bright, M. A., Alford, S. M., Hinojosa, M. S., Knapp, C. & Fernandez-Baca, D. E. Adverse childhood experiences and dental health in children and adolescents. Community Dent. Oral Epidemiol. 43, 193–199 (2015).
20. Burke, N. J., Hellman, J. L., Scott, B. G., Weems, C. F. & Carrion, V. G. The impact of adverse childhood experiences on an urban pediatric population. Child Abuse Negl. 35, 408–413 (2011).
21. Flaherty, E. G. et al. Adverse Childhood Experiences and Child Health in Early Adolescence. JAMA Pediatr. 167, 622–629 (2013).
22. Jimenez, M. E., Wade, R., Schwartz-Soicher, O., Lin, Y. & Reichman, N. E. Adverse Childhood Experiences and ADHD Diagnosis at Age 9 Years in a National Urban Sample. Acad. Pediatr. 17, 356–361 (2017).
23. Kerker, B. D. et al. Adverse Childhood Experiences and Mental Health, Chronic Medical Conditions, and Development in Young Children. Acad. Pediatr. 15, 510–517 (2015).
24. Mersky, J. P., Topitzes, J. & Reynolds, A. J. Impacts of adverse childhood experiences on health, mental health, and substance use in early adulthood: A cohort study of an urban, minority sample in the U.S. Child Abuse Negl. 37, 917–925 (2013).
25. Pretty, C., O’Leary, D. D., Cairney, J. & Wade, T. J. Adverse childhood experiences and the cardiovascular health of children: a cross-sectional study. BMC Pediatr. 13, 208 (2013).
26. Thompson, R. et al. Trajectories of Adverse Childhood Experiences and Self-Reported Health at Age 18. Acad. Pediatr. 15, 503–509 (2015).
27. Caballero, T. M., Johnson, S. B., Buchanan, C. R. M. & DeCamp, L. R. Adverse Childhood Experiences Among Hispanic Children in Immigrant Families Versus US-Native Families. Pediatrics e20170297 (2017). doi:10.1542/peds.2017-0297
28. Llabre, M. M. et al. Childhood Trauma and Adult Risk Factors and Disease in Hispanics/Latinos in the US: Results From the Hispanic Community Health Study/Study of Latinos (HCHS/SOL) Sociocultural Ancillary Study. Psychosom. Med. 1 (2016). doi:10.1097/PSY.0000000000000394
29. Wing, R., Gjelsvik, A., Nocera, M. & McQuaid, E. L. Association between adverse childhood experiences in the home and pediatric asthma. Ann. Allergy. Asthma. Immunol. 114, 379–384 (2015).
30. Isasi, C. R. et al. Association of Childhood Economic Hardship with Adult Height and Adult Adiposity among Hispanics/Latinos. The HCHS/SOL Socio-Cultural Ancillary Study. PLOS ONE 11, e0149923 (2016).
31. Campbell, F. et al. Early Childhood Investments Substantially Boost Adult Health. Science 343, 1478–1485 (2014).
32. Perez, N. M., Jennings, W. G., Piquero, A. R. & Baglivio, M. T. Adverse Childhood Experiences and Suicide Attempts: The Mediating Influence of Personality Development and Problem Behaviors. J. Youth Adolesc. 45, 1527–1545 (2016).
33. Martinez, J. I., Gudiño, O. G. & Lau, A. S. Problem-Specific Racial/Ethnic Disparities in Pathways From Maltreatment Exposure to Specialty Mental Health Service Use for Youth in Child Welfare. Child Maltreat. 18, 98–107 (2013).
34. Gudiño, O. G., Lau, A. S., Yeh, M., McCabe, K. M. & Hough, R. L. Understanding Racial/Ethnic Disparities in Youth Mental Health Services: Do Disparities Vary by Problem Type? J. Emot. Behav. Disord. 17, 3–16 (2009).
35. Ramirez, A. Mental Health & Latino Kids: A Research Review. Salud America (2017). Available at: https://salud-america.org/healthymindsresearch/. (Accessed: 29th September 2017)
36. Ramos-Olazagasti, M. A., Bird, H. R., Canino, G. J. & Duarte, C. S. Childhood Adversity and Early Initiation of Alcohol Use in Two Representative Samples of Puerto Rican Youth. J. Youth Adolesc. 46, 28–44 (2017).
37. Allem, J.-P., Soto, D. W., Baezconde-Garbanati, L. & Unger, J. B. Adverse childhood experiences and substance use among Hispanic emerging adults in Southern California. Addict. Behav. 50, 199–204 (2015).
38. Walsh, E. G. & Cawthon, S. W. The mediating role of depressive symptoms in the relationship between adverse childhood experiences and smoking. Addict. Behav. 39, 1471–1476 (2014).
39. Robert Wood Johnson Foundation. Traumatic Experiences Widespread Among U.S. Youth, New Data Show. RWJF (2017). Available at: https://www.rwjf.org/en/library/articles-and-news/2017/10/traumatic-experiences-widespread-among-u-s–youth–new-data-show.html. (Accessed: 25th October 2017)
By The Numbers
142
Percent
Expected rise in Latino cancer cases in coming years