Share On Social!
This is part of the Salud America! Achieving a Cohesive Culture for Health Equity in Latino and All Communities: A Research Review»
Implicit Bias Is a Key Mechanism People Use to Excuse Discrimination among People of Color, Those in Poverty
Bias is the tendency to favor one group over another. Most people think they harbor no bias toward other people, or they believe they know their biases and don’t act on them.
The first type of bias is explicit bias, or overt bias.
Explicit bias is a consciously held set of beliefs about a social group. Acting on race or ethnicity-based bias would be conscious, or explicit, racism, which many Americans openly reject, although which still exists in American society.
The second type of bias is implicit bias, or unconscious bias.
Implicit bias is preconceived notions, or stereotypes, which affect our understanding, actions, and decisions about others—and which operate beyond our control. These perceptions play an integral role in our brain processes. Perceptions about people based on socioeconomic status, race, ethnicity, level of education, political leaning, style of dress, etc., lead us to behave a certain way toward that person or group of people, involuntarily.42 Marcelin et al. note that implicit bias influences all human interactions, as our brains use “innate tendencies to categorize everything we encounter” as a shortcut.43
Importantly, implicit biases do not necessarily align with one’s stated beliefs or reflect stances we would explicitly endorse—making us do things we might not consciously support. We generally tend to hold implicit biases that favor our ingroup, though this is not always the case. Significant research has documented that implicit bias has a real-world effect on behavior, with data from various domains including employment, education, and criminal justice, among others.44
 However, research has also demonstrated that implicit biases are malleable, meaning these unconscious associations can be “unlearned” and replaced with new mental associations.44 Thus, intervention programs aimed at “rewiring” implicit biases in the direction of more compassion and understanding for the impoverished, minorities, and people of color may lead to more equitable distribution of resources and access to health and wealth opportunity.
However, research has also demonstrated that implicit biases are malleable, meaning these unconscious associations can be “unlearned” and replaced with new mental associations.44 Thus, intervention programs aimed at “rewiring” implicit biases in the direction of more compassion and understanding for the impoverished, minorities, and people of color may lead to more equitable distribution of resources and access to health and wealth opportunity.
Many white Americans outwardly oppose explicit racism, though many of those same white Americans harbor implicit prejudices against minorities, perhaps unknowingly or unintentionally perpetuating harmful racist behavior. In fact, most white Americans continue to reside in majority white neighborhoods, sending their children to majority white schools, and, in general, have limited contact with nonwhites. The choice to remain largely segregated from and limit interactions with other racial and ethnic groups serves to bolster racist beliefs and behaviors, whether knowingly or not.12
Implicit Bias Can Unintentionally Perpetuate Inequities in Health
In 2003, the Institute of Medicine published a report stating that “bias, stereotyping, and clinical uncertainty on the part of healthcare providers” contribute to the significant health disparities that exist in the United States across a range of illnesses. The report found that racial/ethnic disparities existed even after adjusting for co-morbidities, socioeconomic differences, and factors affecting access to care, such that they were due in part to bias against minorities, stereotypes about the behavior of minorities, and increased clinical uncertainty when treating minority patients.45 Though explicit racial bias has declined over the past half-century and is considered unacceptable by many, implicit bias persists.46,47
Implicit bias is difficult to overcome, as many health care providers may not believe that they harbor stereotypes that affect how they treat their patients. These implicit stereotypes are generally systematically biased, as a noticeable physical attribute, such as skin color, is used to draw conclusions about other attributes that cannot be seen, such as intelligence, honesty, or compliance. This type of bias cannot be accurately measured via self-report and is instead measured using tools such as the implicit-association test (IAT). The IAT measures the strength with which concepts (in this case, race or ethnicity) are associated with attributes such as good or bad.46,47
Blair et al.46 aimed to measure both implicit and explicit ethnic/racial biases of primary care physicians in the Denver area between May 2009 and May 2010. Explicit bias toward African Americans and Latinos was measured using a feeling thermometer (cool to warm on a scale of 0 to 100) and trait-rating scales (hardworking-lazy, cooperative-hostile, and so on); implicit bias was measured using the IAT.46
 Results of the study showed that, in comparing the group of primary care physicians to the group of community members, the physicians were more likely to be white, fluent in Spanish, and of higher SES. There was weak to non-existent explicit bias expressed toward African Americans or Latinos by either group, but strong implicit bias against Latinos was reported for both physicians and community members, and two thirds of the physicians showed implicit bias that favored whites.46
Results of the study showed that, in comparing the group of primary care physicians to the group of community members, the physicians were more likely to be white, fluent in Spanish, and of higher SES. There was weak to non-existent explicit bias expressed toward African Americans or Latinos by either group, but strong implicit bias against Latinos was reported for both physicians and community members, and two thirds of the physicians showed implicit bias that favored whites.46
In a second analysis by Blair et al.,46 the authors contacted by phone 2,908 patients of 134 of the 210 physician participants from the prior study to have these patients rate their interactions with the physicians using four subscales of the Primary Care Assessment Survey (PCAS) that assessed perceived bias via interpersonal treatment, communication, trust, and contextual knowledge. The majority of the physicians had implicit bias against African Americans and Latinos. Latino patients have comparatively lower ratings of patient centeredness compared to white patients (P < 0.0001), though these low ratings had no association with the clinicians’ racial bias toward Latinos.46
Blendon et al.48 surveyed 4334 U.S. adults in 2007 to study patients’ perceptions of the quality of their care, comparing the perceptions of patients in 14 racial/ethnic groups to the perceptions reported by white patients. Participants were asked questions regarding wait times and quality of patient-provider interactions. Ten out of the 14 racial/ethnic groups, including Mexican-Americans, were significantly less likely to report good or excellent care compared to white patients (P < 0.05).48
López-Cevallos and Harvey23 conducted interviews with Latino young adults living in rural Oregon to assess health care discrimination against the Latino population. The participants were recruited from farms, health clinics, health fairs, and other community locations. In-person computer assisted interviews of approximately one hour were administered by staff members of the Proyecto de Salud Para Latinos program.23 Health care discrimination was measured using a one-item question about personal experiences with discrimination while seeking medical care. In addition, immigration status was determined by asking participants where they were born. The study revealed that foreign-born Latinos were more likely to experience health care discrimination, as were those currently attending school and those with middle and lower incomes. Overall, 39.5% of participants reported healthcare discrimination, compared to 30% of Latinos overall, suggesting that Latinos in rural areas are more likely to experience health care discrimination.23
In a 2015 systematic review of 15 studies that sampled existing health care providers and providers-in-training, all but one study found low to moderate levels of implicit bias among health care professionals, with similar levels of bias toward blacks, Latinos, and “dark-skinned people.”49 Most of these were cross-sectional studies with U.S. participants and assessed implicit bias using the IAT. Implicit bias was found to be significantly related to patient-provider interactions and patient health outcomes, and, to a slightly lesser but still significant degree, treatment decisions. The review found that most providers have implicit bias: that is, positive attitudes toward white patients, and negative attitudes toward patients of color.49
Implicit bias held by health care providers in the United States against Latino and black patients has resulted in significant differences in treatment decisions, as evidenced by several recent studies.50,51 A 2019 meta-analysis of studies published between 1990 and 2018 demonstrated that black patients were 40% less likely and Latino patients 25% less likely to be given analgesia for acute pain relative to non-Latino white patients in United States emergency rooms.50 Similarly, black and Latino patients were less likely to receive mechanical thrombectomy for treatment of acute ischemic stroke relative to white patients (7.0% vs. 9.8%; P < 0.001); this procedure is proven to reduce fatalities and improve patients’ quality of life following a stroke.51 Furthermore, new data show that as resident physicians face burnout, their implicit biases play a larger role in their treatment decisions, placing Latinos and black patients at higher risk for lower-quality health care.52
Combined, these data suggest that any intervention that can reduce implicit bias in the healthcare setting would benefit these populations.
Implicit Bias Interventions in the Health Care Realm
Interventions to decrease implicit bias in the healthcare setting are becoming more readily available, as the problem of implicit bias is more widely recognized.
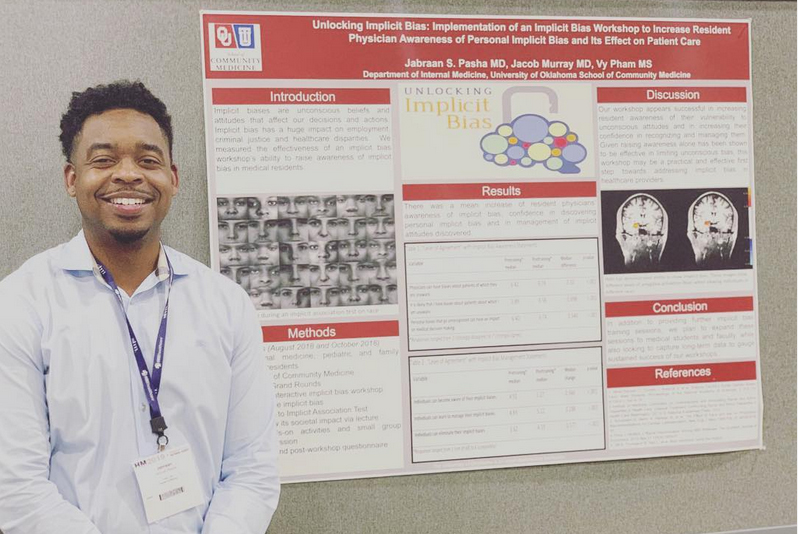
Jabraan Pasha, M.D.,42 and Kelly Capatosto,53 of the Kirwan Institute for Race and Ethnicity at Ohio State University have each developed implicit bias training programs targeting the health care environment.
Both highlight how such programs need to approach the issue of implicit bias without blame or shame, and need to incorporate personal anecdotes that the audience can identify with to make the training relevant.53,54
Pasha’s workshop, “Unlocking Implicit Bias,” is an engaging practical learning experience that is straightforward, compassionate, and empathetic. It incorporates poignant storytelling, events and trends from national headlines, and Pasha’s personal anecdotes featuring his own experience as both the perpetrator and the victim of implicit bias—removing feelings of shame and guilt that many people associate with implicit bias. Importantly, participants then work together to formulate a personalized list of methods to combat implicit bias.54
How You Can Address Implicit Bias
The good news is you can “rewire” implicit bias toward more compassion for others.
Download the free Salud America! “Find Out If You Have Implicit Bias and What to Do Next” Action Pack. This will guide you to see if you have implicit bias, learn from others who have overcome their own implicit bias, and encourage others to learn about implicit bias, too.
The Action Pack was created by Dr. Amelie G. Ramirez, director of Salud America! at UT Health San Antonio.
See the full guide on implicit bias »
See the full guides on the other key mechanisms of discrimination »
See the Guide: Moral Disengagement!
See the Guide: System Justification!
More from our Research Review »
- Introduction/Methods
- Research: Poverty among Latinos
- Research: Rural Poverty
- Research: Poverty and Healthcare
- Research: Discrimination and Education
- Research: Discrimination and Outcomes
- Mechanism: Implicit Bias
- Mechanism: System Justification
- Mechanism: Moral Disengagement
- Strategy: Intergroup Contact Theory
- Strategy: Peer Modeling
- Strategy: Implicit Bias Training
- Strategy: Effective Communication
- Strategy: Social Media for Social Change
- Strategy: Building Social Cohesion
- Policy Implications
- Future Research
References for this section »
12. Asante-Muhammad D. Racial Wealth Snapshot: Latino Americans. Prosperity Now. https://prosperitynow.org/blog/racial-wealth-snapshot-latino-americans. Published 2018. Accessed June 11, 2020.
23. López-Cevallos DF, Harvey SM. Foreign-Born Latinos Living in Rural Areas are more likely to Experience Health Care Discrimination: Results from Proyecto de Salud para Latinos. J Immigr Minor Heal. 2016;18(4):928-934. doi:10.1007/s10903-015-0281-2
42. Salud America!, Cantu-Pawlik S. What is Implicit Bias and Why Should You Care? https://salud-america.org/what-is-implicit-bias-and-why-should-you-care/. Published 2019. Accessed June 11, 2020.
43. Marcelin JR, Marcelin JR, Siraj DS, Victor R, Kotadia S, Maldonado YA. The Impact of Unconscious Bias in Healthcare: How to Recognize and Mitigate It. J Infect Dis. 2019;220(2):262-273. doi:10.1093/infdis/jiz214
44. Staats C, Capatosto K, Tenney L, Mamo S. State of the Science Implicit Bias Review. http://kirwaninstitute.osu.edu/implicit-bias-training/resources/2017-implicit-bias-review.pdf. Accessed June 17, 2020.
45. Institute of Medicine Committee on Understanding and Eliminating Racial and Ethnic Disparities in Health, Smedley B, Stith A, Nelson A. Unequal Treatment: Confronting Racial and Ethnic Disparities in Health Care.; 2003. https://www.ncbi.nlm.nih.gov/books/NBK220355/. Accessed June 18, 2020.
46. Blair I V, Havranek EP, Price DW, et al. Assessment of biases against Latinos and African Americans among primary care providers and community members. Am J Public Health. 2013;103(1):92-98.
47. James S. The strangest of all encounters: racial and ethnic discrimination in US health care. Cad Salude Publica. 2017;33(1). doi:10.1590/0102-311X00104416
48. Blendon RJ, Buhr T, Cassidy EF, et al. Disparities In Physician Care: Experiences And Perceptions Of A Multi-Ethnic America. Health Aff. 2008;27(2). doi:10.1377/hlthaff.27.2.507
49. Hall WJ, Chapman M V., Lee KM, et al. Implicit racial/ethnic bias among health care professionals and its influence on health care outcomes: A systematic review. Am J Public Health. 2015;105(12):e60-e76. doi:10.2105/AJPH.2015.302903
50. Lee P, Le Saux M, Siegel R, et al. Racial and ethnic disparities in the management of acute pain in US emergency departments: Meta-analysis and systematic review. Am J Emerg Med. 2019;37(9). doi:10.1016/j.ajem.2019.06.014
51. Rinaldo L, Rabinstein AA, Cloft H, Knudsen JM, Castilla LR, Brinjikji W. Racial and Ethnic Disparities in the Utilization of Thrombectomy for Acute Stroke: Analysis of Data from 2016 to 2018. Stroke. 2019;50(9):2428-2432. doi:10.1161/STROKEAHA.118.024651
52. Dyrbye L, Herrin J, West CP, et al. Association of Racial Bias with Burnout among Resident Physicians. JAMA Netw Open. 2019;2(7). doi:10.1001/jamanetworkopen.2019.7457
53. West H, Capatosto K. Kelly Capatosto: Shedding New Light on Implicit Bias | Salud America. https://salud-america.org/kelly-capatosto-shedding-new-light-on-implicit-bias/. Published 2019. Accessed June 12, 2020.
54. Cantu S, Pasha J. Dr. Jabraan Pasha: Tearing Down Implicit Bias in the Doctor’s Office | Salud America. https://salud-america.org/dr-jabraan-pasha-tearing-down-implicit-bias-in-the-doctors-office/. Accessed June 12, 2020.
By The Numbers
3
Big Excuses
people use to justify discriminatory behavior