Share On Social!
We all know that some viruses make us sick, like norovirus, which causes vomiting and diarrhea; rhinovirus, which causes the common cold; and SARS-CoV-2, the virus that causes COVID-19.
But how do these viruses make us sick? What happens when a virus gets into the body?
Our bodies are made up of billions of microscopic building blocks, called cells.
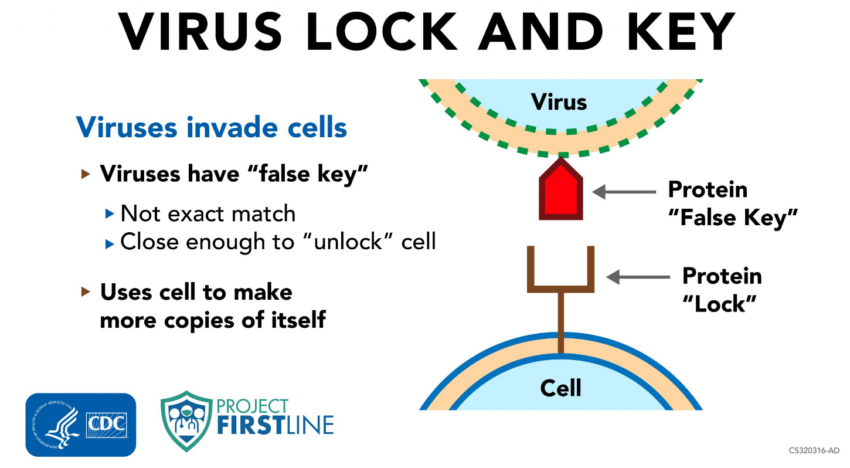
On the outside of our cells, there are tiny parts that stick out. Those tiny parts are made of proteins that act like a lock on a door. If you have the right “key” for the “lock,” then you can get into the cell.
Some virus cells can have tiny parts that stick out on their outsides, too. Those tiny parts can work like a “false key” that can fit the “lock” to some types of our bodies’ cells. It’s not an exact match, but it’s close enough that the virus can get into the body’s cell.
“When a virus gets inside, it ‘hijacks’ the machinery of the cell and uses it to make more copies of itself, including more copies of that false key,” said Dr. Abigail Carlson, an infectious diseases physician with the Centers for Disease Control & Prevention (CDC), as part of CDC Project Firstline’s Inside Infection Control video series. “Those new virus copies with their false keys break out of those infected cells and move on to infect new cells, and in many cases, the cell that’s been infected and hijacked is destroyed in the process.”
What Happens When Viruses Get Into Our Cells?
When enough virus has been able to get into enough of our cells and make copies of themselves, we start feeling sick and have symptoms like fever, chills, and cough.
Symptoms occur because our body recognizes that there is an infection and sends out an alarm to the immune system to begin fighting off the virus. 
“It is this activity of our immune system getting to work that makes us feel sick,” said Dr. Carlson.
Sometimes, our immune system can fight a virus without us feeling sick. When that happens, it’s still possible to spread virus to others.
For instance, if you are infected with a respiratory virus – like SARS-CoV-2 or the flu – but you don’t feel sick, your respiratory droplets can still have virus in them. When you cough, breathe out, or talk, those droplets are carried out and can get in someone else’s nose, throat, lungs, or eyes.
Then the virus cells can start the process of using their false keys to take over the body’s cells and make copies of themselves. That’s why a lot of our infection control actions for respiratory illnesses, like COVID-19, focus on keeping respiratory droplets out of the air and away from people.
Knowing how viruses make us sick can help us understand the actions we take for infection control in hospitals, nursing homes, and other healthcare settings.
What Can You Do to Promote Infection Control in Your Healthcare Setting?
Access more information about infection prevention and control in healthcare by visiting resources from CDC Project Firstline.
Project Firstline creates resources, including videos and shareable images, web buttons, posters, and print materials. They also have facilitator toolkits to help workers lead trainings even if they are not an infection control expert.
Salud America! at UT Health San Antonio is working with the National Hispanic Medical Association to bring Project Firstline infection control educational content to healthcare workers, so they are equipped with the knowledge they need to protect themselves, their facilities, and their patients (Latinos and all communities) from infectious disease threats in healthcare settings.
You can read these articles:
- What is Project Firstline?
- What’s a Virus?
- How Does Infection Control Work on COVID-19 Variants Like Omicron?
- Contact Time: What is It and How Does it Impact Infection Control?
- The Surprising Difference Between Cleaning and Disinfection
- What’s a Respiratory Droplet and Why Does It Matter?
- Why Do Cleaning and Disinfection Matter in Healthcare?
- We Need to Talk about Hand Hygiene Again
- What is the Goal of Infection Prevention and Control in Healthcare Settings?
- The Intersection of Infection Prevention and Control and Healthcare Equity
- N95 Respirators: Everything You Need to Know
- How Do I Safely Use a Multi-Dose Vaccine Vial?
“Healthcare teams in hospitals, nursing homes, and other care settings are the front lines against the spread of infection,” said Dr. Amelie G. Ramirez, director of Salud America! at UT Health San Antonio. “CDC’s Project Firstline is bolstering those efforts by developing evidence-based tools that can be delivered in a variety of ways to make infection control learning convenient and accessible for busy healthcare staff.”
LEARN MORE ABOUT PROJECT FIRSTLINE!
Editor’s Note: This article is part of a collaboration between Salud America!, the National Hispanic Medical Association, and the CDC’s Project Firstline. To find resources training materials, and other tools to bolster knowledge and practice of infection control, visit Project Firstline and view Salud America!’s infection control content.
By The Numbers
142
Percent
Expected rise in Latino cancer cases in coming years



[…] The pandemic is another chapter in the bitter story of American racism and inequality. Black and Latinx people are being infected and are dying at much higher rates than white Americans. Many people of […]
[…] coronavirus has killed over 61,000 Latinos in America according to the CDC, accounting for over 18.2% of the total COVID deaths in the […]
[…] Whereas Hispanics make up 11% of D.C.’s inhabitants, they signify 19% of the COVID cases, and 14% of the deaths. Equally, 46% of D.C.’s residents are Black, they usually make up an alarming 75% […]
[…] and historical mistreatment. According to the U.S. Centers for Disease Control and Prevention, Latino and Black American communities are three times more likely to become infected with […]
[…] Covid pandemic has hit the Latino community particularly hard, and data from the nonprofit health equity advocacy group Salud America! shows Latinos lead in the 0-24 age […]
[…] the pandemic, Latinos took major blows, both in terms of COVID-19 cases and also from the economic recession under former President Donald Trump. Nearly half (49%) of […]
[…] the positive trend, the harm may have already been done. The pandemic has disproportionately impacted Latino communities. Reuters reported that election-related or political disinformation that […]
[…] pesar de la tendencia positiva, es posible que el daño ya esté hecho. La pandemia ha impactado desproporcionadamente Comunidades latinas. Reuters informó que la desinformación política o relacionada con las […]
[…] residentes blancos muestran una tasa mucho más baja con 10 muertes por cada 100,000 habitantes(8 9) . Los afroestadounidenses por su parte, denuncian subsistemas de salud que les segregan […]
[…] https://salud-america.org/coronavirus-case-rates-and-death-rates-for-latinos-in-the-united-states/ […]
[…] https://salud-america.org/coronavirus-case-rates-and-death-rates-for-latinos-in-the-united-states/ […]
[…] communities have the second-highest number of COVID-19 cases in the U.S. They’re also more likely to become hospitalized and die from the disease than other […]
[…] total, around 160,000 Latinos were killed by COVID-19. This accounts for 16% of the 1 million deaths in the country. The […]