
Share On Social!
Spending on health is rising in America.
Yet, ironically, health outcomes are getting worse. In fact, people here experience the worst health outcomes overall of any high-income nation.
U.S. residents are more likely to die younger, and from avoidable causes, than residents of peer countries, according to a 2023 report from The Commonwealth Fund.
Let’s compare health outcomes with peer countries to provide an important baseline for where we are in health outcomes and set a target for where we could be.
The U.S. and 5 Important Domains of Healthcare Systems
A 2021 study by The Commonwealth Fund compared five performance domains of health care systems across 11 high-income countries.
Researchers found the U.S. ranks last on four of five domains:
- access to care (last)
- administrative efficiency (last)
- equity (last)
- health care outcomes (last)
- care process
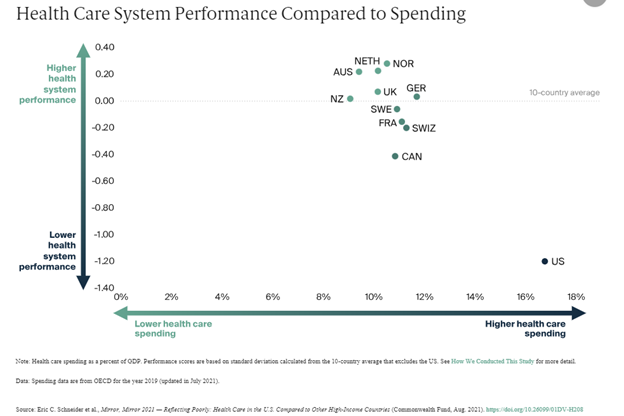
This is despite that the U.S. spends a far greater share of its gross domestic product on health care than other high-income nations.
The U.S. didn’t just rank low, either. It performed so far below other countries that it was a substantial outlier and negatively skewed the mean performance.
For example, “the U.S. rate of 17.4 [maternal] deaths per 100,000 live births is twice that of France, the country with the next-highest rate (7.6 deaths per 100,000 live births),” the study found.
Although the study focused on specific health care outcomes that are influenced by the delivery of medical services, the authors acknowledge that health outcomes are influenced by non-medical factors outside the control of health care systems.
“Policies and public investments in education, employment, nutrition, housing, transportation, and environmental safety shape the health of the population,” the study states.
Because the health landscape is continually shifting with growing research on medical devices and these non-medical factors, comparing outcomes with peer countries is also important to shed light on the best non-medical practices behind why some countries might be more successful than others.
The U.S. and Non-Medical Factors (the Social Determinants of Health)
Non-medical factors are the conditions we are born, grow, live, work, play, and age. They are known as social determinants of health (SDoH).
Globally, improvements in SDoH over the past 100 years have contributed to improvements in health. The drastic differences we see in health outcomes and life expectancy across nations today are largely explained by differences in SDoH.
Due to past and present discriminatory policies and practices in America, which originated in overt racism and continue to be reinforced by overt classism, not all communities were created equal.
Rather, there are large differences in SDoH within and between U.S. cities.
While some Americans benefit from good conditions, other Americans are burdened by poor conditions. They may face unequal distribution of power and resources, unaffordable childcare, unstable housing, limited employment opportunities, income inequality, unhealthy food, insufficient parks, unsafe streets, and inadequate transportation options.
In the 2021 study by The Commonwealth Fund, researchers considered these non-medical SDoH factors as potential reasons why other high-income countries are outperforming the U.S. in health outcomes.
They found that, compared to poorer-performing countries, top-performing countries invest in these non-medical conditions.
“[Other nations] invest in social services that increase equitable access to nutrition, education, child care, community safety, housing, transportation, and worker benefits that lead to a healthier population and fewer avoidable demands on health care,” according to the study.
For the U.S. to attain better and more equitable health outcomes, we need to invest in these non-medical conditions, particularly in disadvantaged communities.
Two strategies to better understand these non-medical conditions are for community advocates to download and share our Health Equity Report Card and for health care providers to screen patients for their non-medical needs, known as SDoH screening.
The Need for SDoH Screening
SDoH screening can help medical providers better understand those social needs and their root causes.
An SDoH screening tool is a questionnaire that gathers information from patients about their general social needs in addition to their immediate health needs.
When patients are screened for social needs at their medical appointments, healthcare providers can identify ways to address those needs and their root causes.
“Health systems can benefit by understanding the social determinants in the communities in which their patients live,” according to the Agency for Healthcare Research and Quality. “In addition to giving them insights into the lived experiences of their patients, health systems that learn about the SDoH of the communities they serve may become inspired to engage in community-level efforts to address those SDoH, such as establishing farmers markets in food deserts, safe exercise space, or affordable housing.”
In this way, SDoH screening has the power to identify and address the causes of social needs which can dramatically improve patient health outcomes.
For instance, let’s look at unreliable transportation.
A 2022 study on more than 56,000 Medicare Advantage beneficiaries explored the relationship between health-related social needs and hospital stays and emergency department visits.
The study found that unreliable transportation had the largest significant association with increased hospital stays and emergency department visits compared to other health-related social needs (financial strain, housing insecurity, poor housing quality, food insecurity, utility insecurity, loneliness, etc.).
Addressing unreliable transportation among this population could reduce hospital stays and emergency department visits.
SDoH screening is key to tackling an issue like this.
See how Nemours Children’s Health and federally qualified health centers are using SDoH screening.
“Health is far more than what can be provided in a doctor’s office,” said Dr. Amelie Ramirez, director of Salud America! and its home base, the Institute for Health Promotion Research at UT Health San Antonio. “In the same way that a team of doctors develops a patient treatment plan to treat cancer, a team of doctors and community services should develop a patient treatment plan that includes addressing social risks and social needs.”
What Can You Do for SDoH
You can help address the non-medical, or SDoH, factors in health outcomes, too.
Download and share a Health Equity Report Card by Salud America! at UT Health San Antonio to compare non-medical factors in your county to the rest of your state and nation.
The Health Equity Report Card auto-generates Latino-focused and local data with interactive maps and comparative gauges, which can help you visualize and explore local inequities in housing, transit, poverty, health care, food, education, and more.
You can email your Health Equity Report Card to local leaders to stimulate action to address these non-medical conditions, particularly in disadvantaged communities.
Use the data in your communication materials or share on social media to raise awareness about the importance of investing in non-medical factors to improve health.
Get your Health Equity Report Card!
Explore More:
Healthcare AccessBy The Numbers
25.1
percent
of Latinos remain without health insurance coverage



