
Share On Social!
Early childhood adversity like abuse and divorce is a root cause of many of the greatest public health challenges we face today.
But doctors don’t even screen children for exposure to adversity.
That’s changing in California, thanks to Dr. Nadine Burke Harris and other child advocates.
As of Jan. 1, 2020, almost 100,000 physicians in 8,800 clinics will be reimbursed for routinely screening Medi-Cal patients for adverse childhood experiences (ACEs), in an effort California hopes will help prevent ongoing ACEs-related stress and disease.
Here are nine big questions surrounding the change.
1. What Is Childhood Adversity (ACEs) and its Impact?
Adverse childhood experiences (ACEs) include abuse, neglect, divorce, parental incarceration, parental mental illness, etc.
These are threatening experiences. These are more than painful memories.

ACEs can trigger a child’s biological stress response. That stress response becomes toxic when it goes without nurturing protection from a stable adult, known as buffering.
Toxic stress leads to activation of the immune and inflammatory systems; changes in brain structure; elevation of blood pressure and blood sugar; changes in how genes are read; and inhibition of the prefrontal cortex, which is responsible for attention, judgement and impulse control.
High levels of stress hormones in the early years can alter a child’s brain and body increasing their risk for:
- heart disease
- cancer
- asthma
- stroke
- Alzheimer’s
- diabetes
- suicide
- teen pregnancy
- substance use disorder
- chronic absenteeism
- dropping out of high school
- involvement in the criminal justice system
ACEs are even linked to teen obesity.
“Our results imply that child health professionals should understand the relationship between ACEs and weight status in adolescence, and that screening for ACEs and referring youth and their families to appropriate services might be an important part of clinical weight management,” according to the researchers who linked ACEs to obesity.
2. Why Is Screening for ACEs So Important?
In California (39.3% Latino), 62.5% of adults have experienced at least one ACE. Nearly 18% have experienced four or more ACEs.
The total economic burden for lifetime costs associated with child maltreatment in California, for example, was $19.3 billion, according to advocacy group Safe and Sound.
By preventing and treating childhood adversity, the nation could save between $124 billion and $585 billion in lifetime costs for each year’s worth of new cases of childhood adversity, according to a 2011 CDC study.
Screening is one of the most basic tools of modern public health and preventive medicine.
Consider infant screenings for phenylketonuria (PKU) and cystic fibrosis; annual screenings for blood pressure; and periodic screenings for certain types of cancer.
ACEs screenings exist, too. They can help providers assess a patient’s risk of a toxic stress physiology. Screening is critical to prevent and treat childhood adversity.
But few have implemented it. No states reimburse doctors who do it.
3. Who Pushed California to Become a Leader in ACEs Screenings?
Today, Nadine Burke Harris is the Surgeon General of California.
Back in 2013, she shined a spotlight on ACEs when she founded the Center for Youth Wellness (CYW). CYW aimed to push pediatric medicine to consider the “biology of adversity” and evaluate ACEs and toxic stress as a root causes of adverse health outcomes in California.

Steered by the CYW, the California Campaign to Counter Child Adversity (4CA) has been a leader in advocating for universal ACEs screening.
Members of 4CA meet with organizations, assembly members and community members to raise awareness of childhood adversity and the need for investment in training and resources for universal screening.
“We need to support the effective implementation of the ACEs screening program by educating our policymakers and advocating for screening coupled with (1) provider training, resources and guidance, (2) care coordination and referral systems, and (3) provider supplemental payments for ACEs screening,” according to a 4CA committee statement to members.
4. How Did California Conceptualize its ACEs Screening?
One method C4A explored to require ACEs screening was through the Early and Periodic Screening, Diagnosis, and Treatment (EPSDT) benefit.
Under federal law, EPSDT provides for periodic screening services for children under age 21 who are enrolled in Medicaid.
- Early: Assessing and identifying problems early
- Periodic: Checking children’s health at periodic, age-appropriate intervals
- Screening: Providing physical, mental, developmental, dental, hearing, vision, and other screening tests to detect potential problems
- Diagnostic: Performing diagnostic tests to follow up when a risk is identified, and
- Treatment: Control, correct or reduce health problems found
The goal of the EPSDT benefit is to ensure these individuals get age-appropriate screening, preventive services, and treatment services that are medically necessary to correct or ameliorate any identified conditions.
In order for Medicaid to cover “other services” not available under the EPSDT benefit, the services must be recognized under state law and be included in the state plan, according to EPSDT – A Guide for States.
4CA wanted to ensure ACEs screening would be recognized under California state law and be included in the Medi-Cal plan within the EPSDT benefit.
However, due to the state’s confusing medical necessity standards, many health providers were denying children access to services they should be receiving.
Even if ACEs screening was added to a list of medically necessary services within EPSDT, many were concerned that providers would not understand—and thus not administer—the screening.
5. How Did California Change State Law to Pave Way for ACEs Screening?
Two changes could help accomplish universal ACEs screening for children enrolled in Medi-Cal:
- Amend the state’s definition of medical necessity and ensure health plans comply with and health providers understand the medical necessity standard; and
- Update services covered within EPSDT to include ACEs screening.
In 2017, the California Legislature passed Senate Bill 1287 (SB 1287), establishing a definition for medically necessary services for individuals younger than 21 and promoting consistent evaluation tools.
The same year, the Legislature also passed Assembly Bill 340 (AB340), which calls for a trauma screening advisory group to update, amend, or develop tools and protocols for screening children for trauma within the EPSDT benefit.
“It’s not about going out and requiring a ton of brand new resources or new money,” said Burke Harris in an interview with The Chronicle of Social Change. “It’s about how do we do a better job of early detection, early intervention and implementing the interventions that we know improve outcomes.”
6. How Did the California Public Influence ACEs Screening?
The Trauma Screening Advisory Group convened state staff, legislative staff, county mental health experts, managed care plan experts, behavioral health experts, child welfare experts, and other stakeholders four times in 2018.
In January 2019, the advisory group submitted its recommendations to the California Department of Health Care Services (DHCS) and the Legislature.
The advisory group evaluated multiple existing tools and programs and recommended allowing Medi-Cal providers to select one of the following three options of how they’ll screen children for ACEs:
- the Pediatric ACEs and Related Life-events Screener (PEARLS) tool;
- the Whole Child Assessment tool;
- and a tool that meets the same criteria as the PEARLS tool.
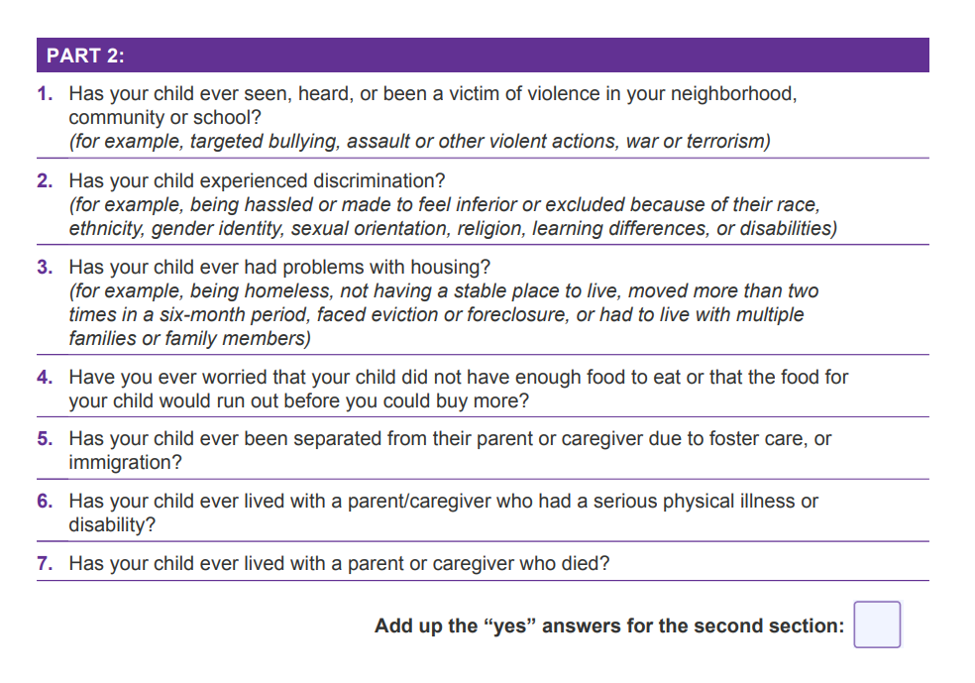
The PEARLS tool was developed by pediatricians and researchers from UCSF Benioff Children’s Hospital Oakland, the UCSF School of Medicine, and the CYW. It is more comprehensive than the orginal ACEs assessment because it includes seven additional questions exploring community violence, discrimination, food insecurity, foster care, immigration, and caregivers with physical illness or disability.
The Whole Child Assessment (WCA) too was developed by Dr. Ariane Marie-Mitchell and colleagues at Loma Linda University. They combined the ACEs questionairre with the required Staying Healthy Assessment (SHA).
The Department of Health Care Services (DCHS) proposed only the PEARLS tool to be eligible for reimbursement in pediatrics and solicited public comments.
Some child health advocates are disappointed that reimbursement is limited to only one tool for children, according to ACEs Connection who obtained the comments through a public information request.
“If we have mandated legislation that only looks at one screening tool, it really limits the opportunity to improve that screening tool over time and it also doesn’t take into consideration that there are a number of tools that are applicable and work really well right now,” said Dr. Kate Williamson, a pediatrician in private practice in Ladera, Calif, according to ACEs Connection.
DCHS is currently working to translate the PEARLS tool into other languages.
The advisory group also encouraged the Legislature to explore systems that support trauma screening for adults, particularly adults in the Medi-Cal system, due to the “intergenerational impact their trauma has on today’s children.”
7. How Did California Pay to Train Primary Care Providers in ACEs Screening?
When Burke Harris become California’s Surgeon General in January 2019, she and 4CA continued advocating for resources to train providers to implement ACEs screening through the California Department of Health Care Services (DHCS) Trauma Screenings proposal, known as Proposition 56.
“I believe fundamentally that social determinants of health are to the 21st century what infectious diseases were to the 20th century,” Burke Harris said during a Berkeley Public Health event. “In my role as state surgeon general, it’s my intention to lay the infrastructure to ensure that in the state of California we will cut ACEs in half in one generation.”
In June 2019, State Gov. Gavin Newsom approved a $45 million budget item to reimburse state Medicaid providers for screening patients on ACEs and another $50 million to train primary care providers to administer those screenings.
Burke Harris’s job was to work with DHCS to train the almost 100,000 primary care providers on how to screen patients and how to respond with trauma-informed care.
Through the Office of the California Surgeon General, she is working to create a state-wide, data-driven quality improvement collaborative and related infrastructure to share challenges and successes.
She also worked to develop a free, two-hour course that trains Medi-Cal providers on clinical protocols and payment for screening children and adults for ACEs.
8. How Does California’s ACEs Screening Work?
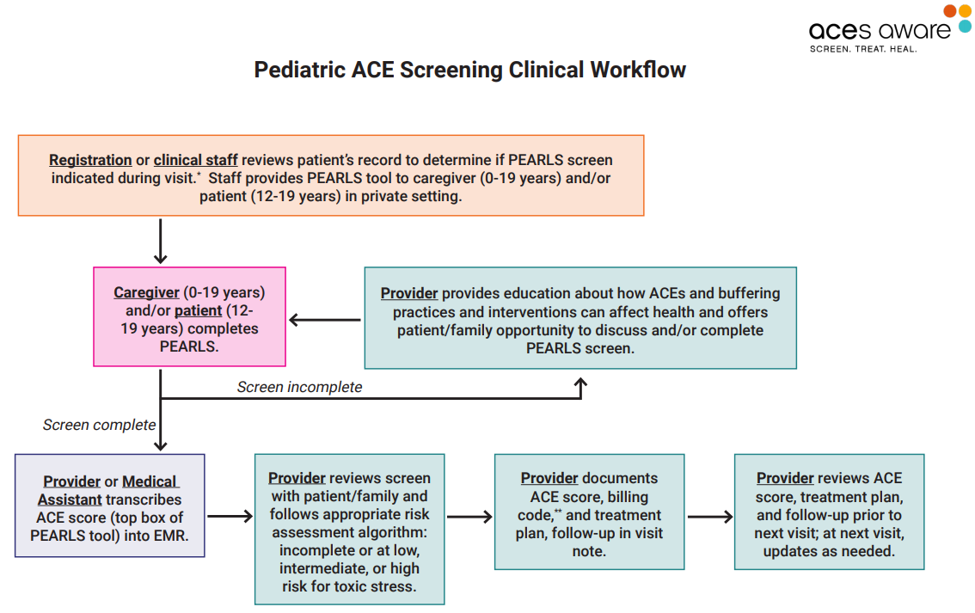
At the beginning of an appointment, the ACEs assessment tool should be given directly to adult patients, caregivers for children and adolescents, and adolescent patients for completion in a private setting.
ACEs assessment tools are available in both identified and de-identified formats. The identified screening tool allows respondents to indicate which of the ACEs categories they or their child experienced. The de-identified screening tool specifies only the total number of ACEs categories that a patient has experienced, not which categories apply.
PEARLs scores include two numbers: one for the traditional ACE score which ranges from 0 to 10; and one for the additional section which ranges from 0 to 7.
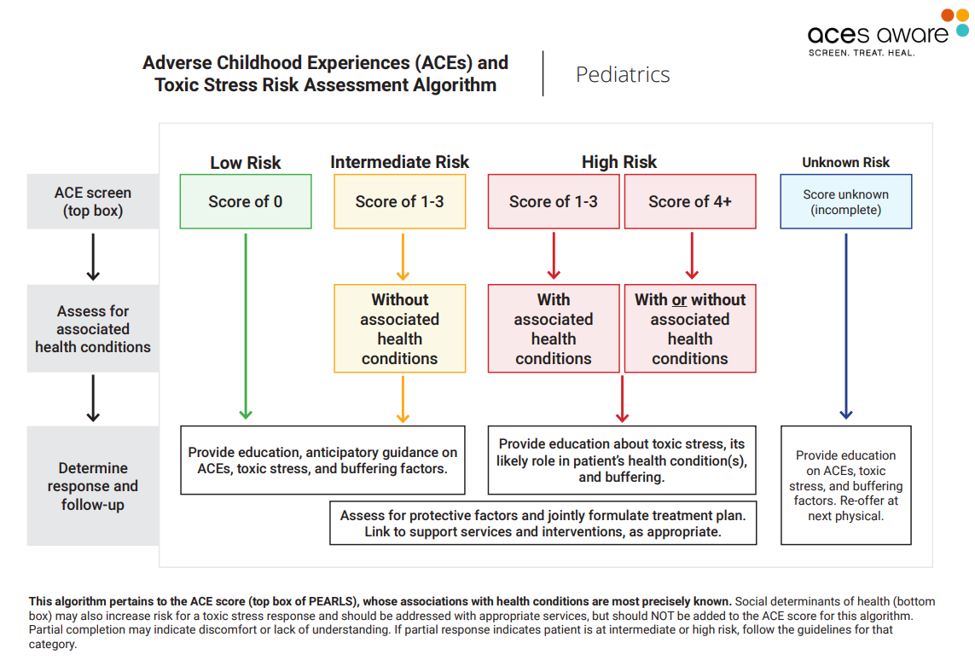
Physicians then use a screening/scoring algorithm to identify children facing low-, intermediate- or high risks of symptoms and health problems associated with ACEs.
When a child is identified as high risk, with or without associated health conditions, the pediatrician will:
- Provide education about toxic stress, its likely role in the patient’s health condition(s), and buffering;
- Assess for protective factors and jointly formulate a treatment plan; and
- Link to support services and interventions, as appropriate.
Beginning Jan. 1, 2020, DHCS began providing a supplemental payment to Medi-Cal providers for conducting ACEs screening for adults and children with Medi-Cal coverage, using Proposition 56 funds. These screenings will be billed and reimbursed in both the managed care and fee-for-service delivery systems.
To bill Medi-Cal, providers use the Healthcare Common Procedure Coding System (HCPCS) billing codes based on the results of the screening. Code G9919 is used for screens that have a score of 4 or greater (high risk) and code G9920 is used for screens that have a score of 0 to 3 (lower risk).
The ACEs Aware website provides information and resources on how to incorporate ACEs screenings into clinical practice, create treatment plans, and deliver trauma-informed care.
“By identifying children who are exposed to adversity early on in life, we can try to reduce their chances of incurring harmful health consequences as adults and support them and their families to achieve better health overall,” said Dr. Dayna Long, director of the UCSF Benioff Children’s Hospital Oakland Center for Child and Community Health. “The state’s support of this tool alongside payments for screening will go a long way to incentivize providers to screen all patients for ACEs.”
Share this with public health and community leaders to start or support universal ACEs screening in your state.
9. What Are the Next Steps to Address ACEs in California?
4CA wants the state to invest even more in prevention, particularly for its most vulnerable children.
“We also need to continue advocating for increased investments in primary prevention strategies that promote and enhance protective factors, including education for parents and caregivers on childhood adversity and toxic stress; strengthen economic support for families; and provide high-quality early education,” according to a 4CA committee statement.
Beyond screenings, Burke Harris wants everyone in education settings and criminal justice to understand the impact stable relationships and environments can have in buffering kid’s toxic stress response.
“Trauma-informed training, practices and policies in the educational setting are fundamental to ensuring that all children have the best opportunity to learn,” she wrote in a statement to the United States House of Representatives Committee on Education and Labor in Sept. 2019.
She also wants primary-care providers to loop school nurses in on the care plan.
“Part of treatment is recognizing that everyone in the educational environment has an opportunity to administer buffering care for kids,” said Burke Harris, according to Patrice Gaines of NBCNews.
How Can You Get Involved in Addressing ACEs?
Even if you’re not in California, you can support children who have experienced trauma.
If you’re a health care provider or school leader, see how this pediatrician started a school-based intervention to provide mental health services to students in need.
If you’re a parent, school leader, or police leader, see how a school-police partnership can help educators and administrators provide stable, nurturing environments and handle students with care in places from San Antonio, Texas, to Nevada, to Moline, Ill.
Download the free Salud America! “Handle With Care Action Pack.” The Action Pack helps police, school, and mental healthcare leaders start the Handle with Care program, in which police notify schools when they encounter children at a traumatic scene, so schools can provide support right away.
By The Numbers
142
Percent
Expected rise in Latino cancer cases in coming years



