
Share On Social!
The steady increase in human average life expectancy in the 20th century is considered one of the greatest accomplishments of public health. A person’s rate of aging has important implications for his/her risk of death and disease.
Now scientists have developed a blood test that reveals how long a person has left to live, The Guardian reports.
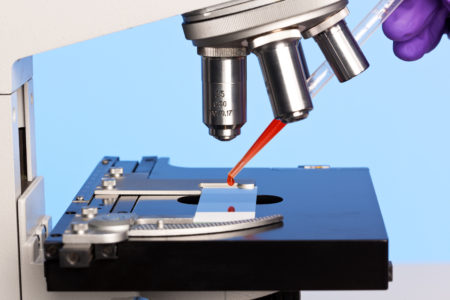
Researchers at Yale School of Public Health used a nationally representative U.S. sample to derive a person’s “Phenotypic Age” based on 34 a linear combination of chronological age and nine multi-system clinical chemistry measures.
The study result suggested that Phenotypic Age is significantly associated with all-cause mortality and cause-specific mortality.
If a person’s phenotypic age is higher than their chronological age, they may be at greater risk of dying.
The risk of dying rose by 14% among those ages 20-39; 10% in those ages 40-65; and 8% among those 65084, if a person’s phenotypic age was above their real age. Overall, people who aged fastest had more diseases than those who aged at a slower pace.
Phenotypic Age is an attractive composite biomarker that captures organismal age and the functional state of many organ systems and tissues, above and beyond what is explained by chronological time.
“We showed that even among people who have no diseases, who are presumably healthy, we can still pick up differences in life expectancy. It’s capturing something preclinical, before any diseases present themselves,” Morgan Levine, a pathologist at Yale, told The Guardian. “It’s picking up how old you look physiologically. Maybe you’re 65 years old but physiologically you look more like a 70 year old, so your mortality risk is more like that of a 70 year old.”
The Yale study shed light on 13 factors that alter the pace of aging, facilitating investigation into potential biological mechanism and 14 environmental stressors. Individuals of the same chronological age may exhibit greatly different susceptibilities to age-related diseases and death due to their health behaviors.
Hence, this study indirectly emphasis the importance of being physically active and eating healthier food.
What the study means to Latinos?
The study has big implications for Latinos.
This is a young population that deals with many health inequities.
For example, Latinos lack of access to places for physical activity, according to a Salud America! research review.
The federal weekly physical activity recommendations for adults are at least 150 minutes of moderate-intensity or 75 minutes of vigorous-intensity aerobic physical activity for substantial health benefits. Still, national data show that fewer than half of the adult U.S. population meets the physical activity recommendations. Latinos have even lower level trends of physical activity.
Latinos also lack of access to healthy food options where they can buy fruits and vegetables, according to a Salud America! research review. Many live in food swamps, too.
These inequities contribute to high rates of obesity and diabetes in this population.
The estimated rate of diabetes, both diagnosed and not diagnosed, is 86 percent higher in the adult Latino population than for non-Latino whites, according to a 2014 CDC report.
Studies also suggest that diabetes contributes to the rising rates of Alzheimer’s in Latinos.
That’s why a blood test, like the one described earlier, is important.
“The biggest advantage of this is now being able to say someone’s at high risk, and that they should come in regularly so you can make sure they’re not developing this or that disease,” Levine told The Guardian.
“It’ll show you how can you reduce their risk because you can plug all the numbers in and see how the risk drops if they bring their glucose down, for example.”
Explore More:
Healthy Families & SchoolsBy The Numbers
142
Percent
Expected rise in Latino cancer cases in coming years



