
Share On Social!
The coronavirus pandemic is weakening the already-fragile rural health care safety net, and endangering health of rural residents, public health experts say.
Here are a few ways this is happening.
The Rural Health Care System and Coronavirus (COVID-19)
Rural hospitals are small businesses that their communities rely upon.
But health staff is becoming sick. Cash-flow problems are at crisis levels, according to the National Rural Health Association.
- Adequate number of supplies and tests
- EMS shortages, as many in rural communities are volunteers;
- Overall workforce shortages if rural providers get sick;
- Telehealth waivers and site flexibility for Rural Health Clinics;
- Critical Access Hospital waivers; and
- Need for loan forbearance
“[We are] receiving on-the-ground reports from rural providers who have grave concerns about their ability to combat COVID-19,” according to the rural organization. “These providers, who were already struggling (48% of rural hospitals currently operate a loss) are reporting significant increases in patient volumes, workforce shortages and significant concerns about access to supplies.”
In Texas, rural hospitals are forced to do layoffs as coronavirus spreads, the Texas Tribune reports.
“Facing critical supply shortages, maxed-out lines of credit, growing payables and disappearing revenue streams, cash-strapped rural Texas hospitals are having to make layoffs to meet payroll,” John Henderson of the Texas Organization of Rural and Community Hospitals told the Tribune. “And this is happening in a moment when we must build and sustain surge capacity.”
Why Are Rural Residents More Vulnerable to Coronavirus?
Age is an issue.
15% of the American population lives in rural areas. This includes 3.2 million Latinos.
Their average age is 73.3.
“This is incredibly bad news when it comes to COVID-19,” reports Forbes. “Being older, as well as having additional health issues have proven considerably more deadly for those who contract the virus.”
Systemic barriers in access to health care are an issue.
Many Latino families lack access to support for quality healthcare, research shows.
In rural communities, due to a shortage of physicians and rural hospitals closing, Latinos and others are even less less connected to emergency health services and life-changing appointments with specialty care doctors.
 These “hospital deserts” have higher rates of poverty and low rates of health education and awareness.
These “hospital deserts” have higher rates of poverty and low rates of health education and awareness.
“One of the most significant contributors to this inequity is the distance between communities,” Salud America! reports. “Since these communities are so isolated, there is no public transportation, which can make doctor appointments and healthy food more readily available.”
Economic barriers are a rural health issue.
Rural workers are less likely to have paid sick leave than urban workers, says the Center for American Progress.
Many work multiple jobs. Or they work jobs that cannot be done remotely.
“For many who live in rural areas, including many communities of color, LGBTQ people, and people with disabilities, these factors make it impossible to work remotely,” according to the report. “Because of the economy that rural Americans face, they do not have the capacity to keep themselves safe from COVID-19 and continue to make a living.”
Even still, Internet access is a problem for one-third of rural homes.
“The lack of broadband services denies any possibility that telehealthcare services could be used during the pandemic in any form both COVID-19 related or otherwise,” reports Forbes.
Just How Vulnerable Are Rural Areas to Serious Cases of Flu and Coronavirus?
Covid-19 may pose the greatest risk to Americans in rural areas if deaths from the coronavirus pandemic are similar to those from the standard flu, according to a new Washington Post data analysis.
Coronavirus is NOT the same as the flu.
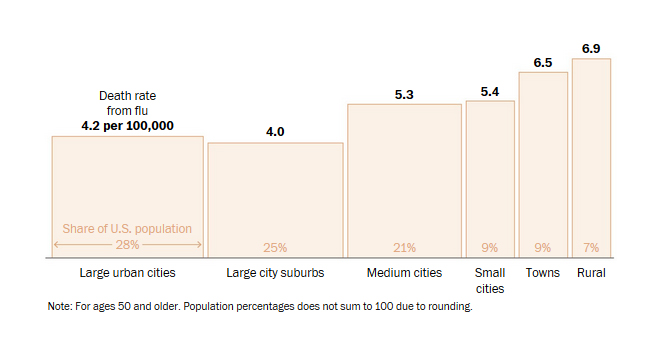
But examining flu death rates for those over age 50 could be a good indicator of vulnerability for Covid-19, says infectious disease specialist Nicholas Reich from the University of Massachusetts.
Rural areas thus are highly susceptible.
“Rural and small city areas in Iowa and Missouri, around the Missouri River and Mississippi River, have had high death rates. Kansas, Nebraska, the Dakotas, Indiana and New England show rates higher than any of the big cities,” the Post reports. “Very rural areas have a 60 percent higher death rate from flu than the big metro areas, according to analysis of CDC death records.”
What Can We Do to Manage Health Care and Prevent Coronavirus in Rural Areas?
The Rural Health Information Hub has an online guide for rural coronavirus response.
“This guide will help you learn about activities underway to address COVID-19,” the website states. “Federal and state agencies, along with national organizations are sharing resources and guidelines to help all communities and healthcare facilities, including rural areas, respond to this issue.”
The National Rural Health Association has a similar coronavirus resource web page.
They also also continue to advocate for rural response with these 14 actions:
- Provide immediate access to capital to ease the cash-flow crisis for rural providers.
- Prioritize access to no-interest loans to small rural health providers.
- Allow immediate and emergency conversion of a rural PPS hospital to a Critical Access Hospital.
- Temporarily adjust Medicare reimbursement rates for all rural providers to 120% of costs, and 130% for rural EMS.
- Suspend Medicare sequester for the duration of the pandemic.
- Utilize federal loan and grant programs for rural providers.
- Update evaluation and management office visit codes to cover those by smartphone (i.e. Facetime,) and at patient location.
- Remove physical, face-to-face requirements from the definition of a clinic visit to provide and bill for telehealth.
- Require the flu and respiratory syncytial virus infection (RSV) test prior to the COVID-19 test.
- Ensure equitable coverage by Medicare, VA, and Medicaid for COVID-19 reimbursements.
- Allocate for federal reimbursement of Medicaid if a state does not allow such coverage.
- Remove licensure barriers.
- Instruct CMS to develop patient surge protections rural hospitals and clinics.
- Review ASPR’s Strategic National Stockpile plans to ensure rural providers will have access.
“We cannot allow access to safety to merely be allocated to those who can pay the most,” says the Center for American Progress. “As policymakers make plans to fight the new coronavirus, rural America must not be left behind.”
What Can You Do to Promote Healthy Environments Where You Live?
Get a “Health Equity Report Card” for Your Area!
 Select your county name and get a customized Health Equity Report Card by Salud America! at UT Health San Antonio. You will see how your area stacks up in housing, transit, poverty, health care, healthy food, and other health equity issues. These compare to the rest of your state and nation.
Select your county name and get a customized Health Equity Report Card by Salud America! at UT Health San Antonio. You will see how your area stacks up in housing, transit, poverty, health care, healthy food, and other health equity issues. These compare to the rest of your state and nation.
You can email your Health Equity Report Card, share it on social media, and use it to make the case for community change to boost health equity.
Get your health equity Report Card!
Editor’s Note: Main image via Civil Eats
Explore More:
AccessBy The Numbers
142
Percent
Expected rise in Latino cancer cases in coming years




