
Share On Social!
Suicide is rising drastically, especially in rural parts of the United States, according to a new study.
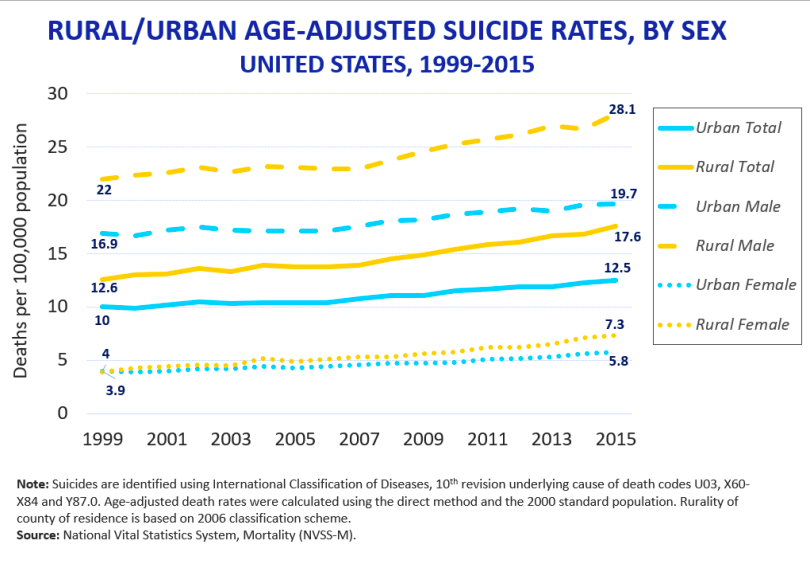
The rate of suicide rose 41% among those ages 25-64 over the past 17 years of data. In addition, suicide rates among people living in rural counties were 25% higher than those in metro areas, NBC News reports.
To reduce these inequities, the Rural Health Information Hub (RHIhub) released a free Rural Suicide Prevention Toolkit.
“The modules in the toolkit contain resources and information focused on developing, implementing, evaluating, and sustaining rural suicide prevention programs,” RHIhub states on their website.
The Issue of Rural Health Care and Suicide
People who live in rural areas face unique health challenges:
- Limited access to primary and mental health care
- Lack of hospitals and pharmacies
- Geographic isolation and housing issues
- Transportation limitations
- Financial constraints. In fact, 40% of rural Americans say they struggle with healthcare, housing, and food expenses, polls show.
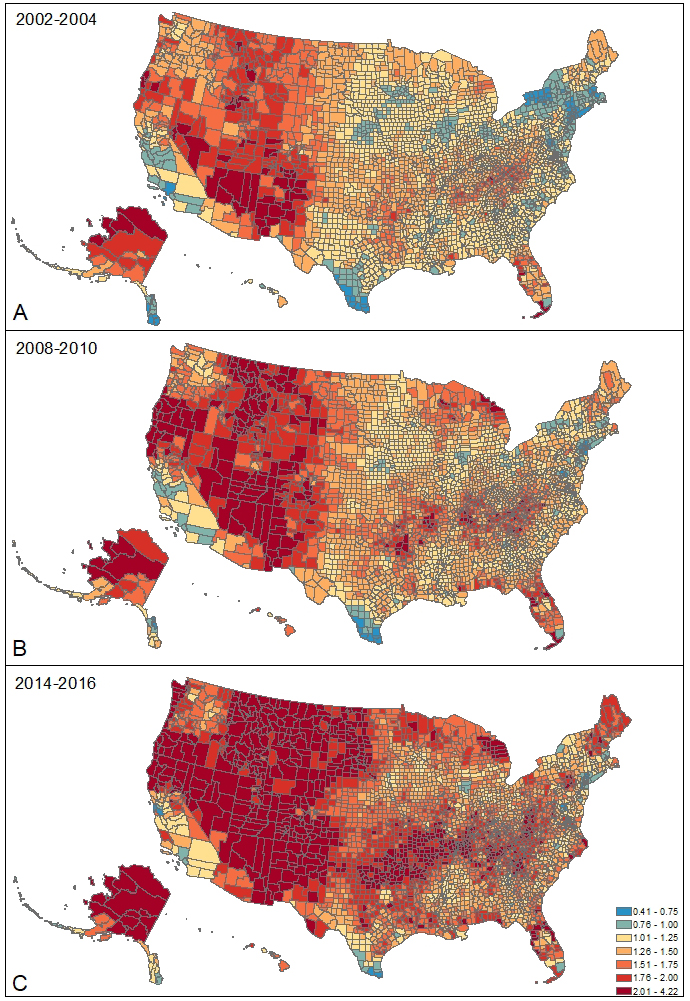
These are the factors driving the rise in rural suicide, according to the new study.
“[Poverty, low income, and underemployment] are really bad in rural areas,” Danielle Steelesmith, study leader from Ohio State University, told NBC News.
However, suicide can be prevented through community action.
That’s why RHIhub created the toolkit with their partners at the NORC Walsh Center for Rural Health Analysis and the University of Minnesota Rural Health Research Center. It was first released in early September 2019.
Exploring How to Prevent Suicide in Rural Communities
RHIhub’s toolkit is broken down into seven modules.
These modules cover background information, community models, potential challenges, and future growth. They also provide resources for both leaders and rural residents for preventing suicide.
Here are the modules to help you create a sustainable suicide prevention program in your rural community.
 Introduction: This module provides an overview of suicide. In addition, it covers challenges unique to rural communities and the impact of suicide on families and friends.
Introduction: This module provides an overview of suicide. In addition, it covers challenges unique to rural communities and the impact of suicide on families and friends.- Program Models: This module introduces program models designed to prevent suicide in rural communities. Multiple approaches are needed to address suicide. Thus, it includes school-based programs, advice for healthcare workers, and training for the community as a whole.
- Program Clearinghouse: A “clearinghouse” is a central office for the collection and spread of resources. The Health Resources and Services Administration (HRSA) has funded several programs in rural areas with the goal of improving rural healthcare. Thus, this module lists a few of these suicide prevention projects and services around the U.S.
- Implementation: Each rural community is unique. There are no one-size-fits-all strategies. Instead, successful programs must adapt to different needs and maximize their resources. Therefore, this module identifies key concepts to keep in mind when starting a prevention program in rural areas.
- Evaluation: Communities need to regularly check that their goals are being achieved. Otherwise, improvements need to be made. This module provides methods and considerations for conducting evaluations of suicide prevention programs.
- Sustainability: Having a sustainability plan helps to ensure that the program continues for a long time. For example, this module includes tips on funding and retention.
- Dissemination: Lastly, wide-spread efforts are essential for the success of rural suicide prevention programs. Sharing results and best practices encourages people in a rural community to learn from their peers.
Other Resources
Living in a rural area is just one risk factor for Latino mental health. For example, housing quality and addiction also have strong impacts on mental health.
If you know someone who is experiencing suicidal thoughts or planning self-harm, there are many resources available to help:
- The National Suicide Prevention Lifeline at www.suicidepreventionlifeline.org or 800-273-TALK
- Veterans Crisis Line – Send a text to 838255
- SAMHSA Treatment Referral Hotline (Substance Abuse) – 1-800-662-HELP (4357)
Addressing social determinants of health is also a big part of the solution.
“You can’t make a dent in these kinds of public health problems without doing something to deal with [those social determinants],” Dr. David Brent, suicide researchers at the University of Pittsburgh, told NBC News. “Yes, you can provide more services to impoverished people, but there’s nothing like helping people get out of poverty.”
Learn more ways to improve mental health for Latinos and all!
Explore More:
Mental HealthBy The Numbers
142
Percent
Expected rise in Latino cancer cases in coming years



