
Share On Social!
It’s no secret that racial bias is prevalent in healthcare settings.
Now, there is more quantitative data to back that sentiment. Research published in JAMA Network Open last May found that as medical residents’ symptoms of burnout, they become more prone to racial bias.
“Rates of burnout symptoms that have been associated with adverse effects on patients, the healthcare workforce, costs, and physician health exceed 50% in studies of both physicians‐in‐training and practicing physicians,” the study states.
“This problem represents a public health crisis.”
Physician Burnout
Physician burnout is a well-known, documented issue.
Workload, pressure, and chaos can significantly contribute to burnout. 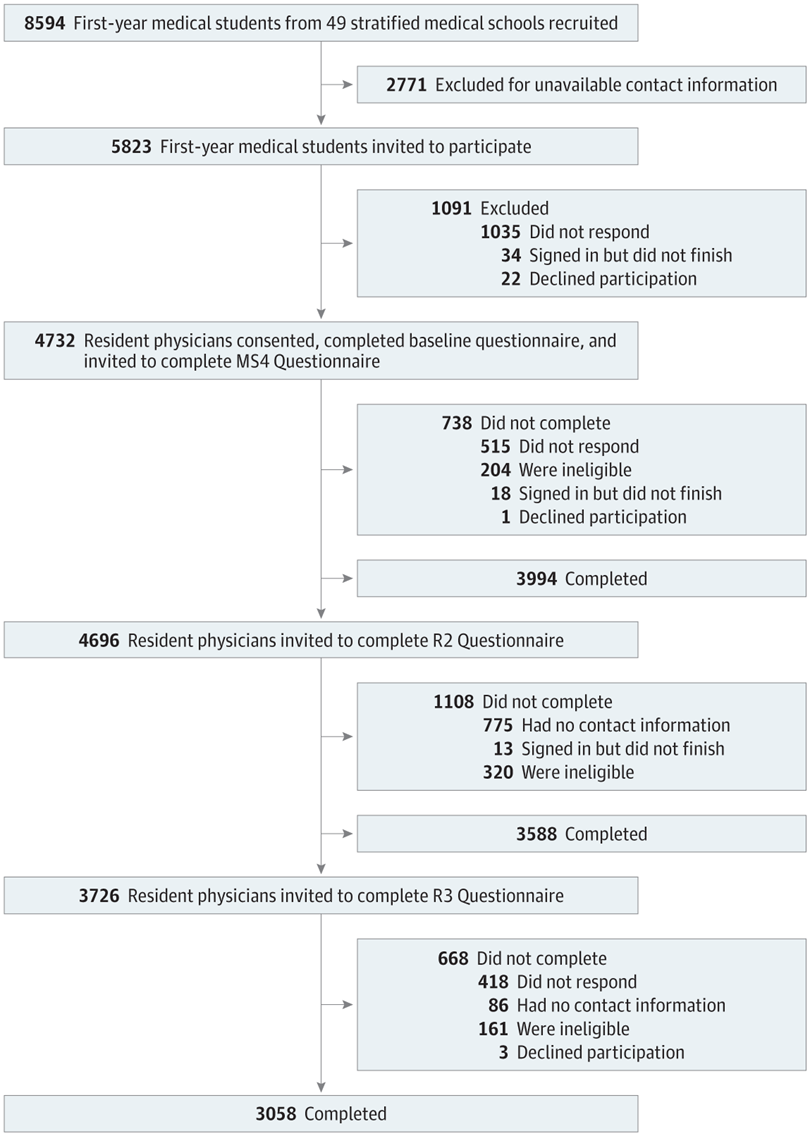
Research has shown that 54% of doctors report feeling burned out. Additionally, doctors suffering from burnout are twice as likely to log significant medical errors.
The suicide rate among physicians is twice that of the general population. It is also one of the highest among all occupations.
Symptoms of burnout amongst physicians include:
- Emotional exhaustion
- Cynicism
- Loss of enthusiasm and joy in their work
- Increasing detachment from their patients
Furthermore, burnout has been linked to higher rates of:
- Depression
- Substance use disorder
- Suicide
To put this into perspective, roughly 4.6 billion is spent yearly due to physician burnout, according to NPR.
Racial Bias & Physician Burnout
Countless studies have shown that physicians—especially white physicians—have implicit preferences for white patients.
This new study further illustrates how there is much more work to do when it comes to implicit biases in health care.
“It’s becoming clearer with each study just how big of a problem this is,” said Liselotte Dyrbye, the study’s lead author and researcher at the Mayo Clinic, told The Washington Post.
The cohort study, published by JAMA, looked at 3392 second-year resident physicians who self-identified as nonblack, symptoms of burnout were associated with greater explicit and implicit racial biases. Recovery from exhaustion in the third year of residency was associated with the most considerable reduction in explicit bias toward black people.
Scientists administered tests for explicit bias by asking residents to rate their feelings toward black or white people on a scale from cold and unfavorable to warm and favorable. The researchers examined implicit bias by asking residents to sort pictures of people of different races along with words like “beautiful,” “cheerful,” “failure,” “scorn” and measuring how rapidly they linked favorable traits to black or white faces.
Among resident physicians, symptoms of burnout appeared to be associated with greater explicit and implicit racial biases; given the high prevalence of exhaustion and the negative implications of bias for medical care, symptoms of burnout may be factored in racial disparities in health care, according to the study.
“No doctor wants to think implicit or explicit bias do play a factor, but we know that for anyone emotions impact behavior and decision. And doctors are not exempt from that,” Dyrbye said.
Harming a patient’s health due to biases based on race, gender, obesity, and other factors are starting to be acknowledged by the medical community.
“When a woman goes into the hospital with chest pain, for example, there are concerns about whether her pain is taken as seriously as a man’s. Whether doctors are going to miss a heart attack because they interpret it as a possible panic attack,” Vineet Arora, a doctor and medical researcher at the University of Chicago, who was not involved in the study but has studied how to improve medical students’ training, told The Washington Post.
Similarly, Latinas and other pregnant women of color face discrimination from healthcare providers. This is due not only due to their race, but also their socioeconomic background.
Solutions to Combat Physician Burnout
Scientists have found that organizational and individual solutions can reduce overall physician burnout symptoms by 10%.
This includes:
ORGANIZATIONAL INTERVENTIONS
- Excessive workload: fair productivity goals, duty-hour limits, and appropriate job role assignments
- Work inefficiency: optimize electronic medical records, shift clerical burdens to non-physician staff, and meet regulatory requirement appropriately
- Work-home balance: respect home responsibilities in scheduling decisions, specify all required work tasks in assigned work hours and support flexible work schedules
- Loss of control: establish work requirements with physician engagement, and promote physician leadership and shared decision-making
- Loss of meaning from work: improve core values, maximize patient time with physicians, foster physician communities, provide professional development opportunities, and offer leadership and awareness training about burnout
INDIVIDUAL INTERVENTIONS
- Excessive workload: consider part-time status, and make informed practice choices to promote efficiency and physician satisfaction
- Work inefficiency: prioritize and delegate tasks appropriately, and attend competence and workplace skills training
- Work-home balance: reflect on life priorities and maintain self-care
- Loss of control: attend stress management training, embrace positive coping strategies, and practice mindfulness
What Can You Do to Address Implicit Bias?
As far as racial bias goes, cultural competency can significantly improve health outcomes as well as reduce the cost of care and inequities.
Additionally, there is a lack of Latinos and other minorities in healthcare professions. Producing more Latino and black doctors are vital to improving healthcare outcomes.
Also, you can take a personal step.
Download the free Salud America! “Find Out If You Have Implicit Bias and What to Do Next” Action Pack. This will guide you to see if you have implicit bias, reflect and learn from others who have overcome their own implicit bias, and encourage others to learn about implicit bias, too.
The Action Pack was created by Dr. Amelie G. Ramirez, director of Salud America! at UT Health San Antonio.
Explore More:
Healthy Families & SchoolsBy The Numbers
142
Percent
Expected rise in Latino cancer cases in coming years



