
Share On Social!
California is leading the nation in addressing toxic stress and adverse childhood experiences (ACEs), such as neglect, divorce and exposure to violence, which can harm long-term health.
Guided by evidence and a public health approach, California developed a series of legal and conceptual frameworks to support statewide screening for ACEs, coordinate within and outside state government, and assess best practices in trauma-informed care across the state.
This progress ramped up when Gov. Gavin Newsom created the Office of the California Surgeon General in 2019 and appointed Dr. Nadine Burke Harris to the position.
In December 2020, Burke Harris released her Roadmap for Resilience: The California Surgeon General’s Report on Adverse Childhood Experiences, Toxic Stress, and Health.
The report covers the science, scope, and impacts of ACEs and toxic stress; public health prevention strategies for multiple sectors; and California’s response to ACEs and toxic stress.
Salud America! is exploring the report as part of its 11-part series on toxic stress.
“A key aspect of California’s strategy for reducing ACEs and toxic stress by half in a generation is recognition of the toxic stress response as a health condition that is amenable to treatment,” the report states.
California’s Response: Support Statewide Screening for ACEs
Screening for ACEs can enable more effective referrals, guidance, and support around preventing and addressing cumulative risk for toxic stress.
California began reimbursing for screening for ACEs in 2020.
“As of Jan. 1, 2020, almost 100,000 physicians in 8,800 clinics will be reimbursed for routinely screening Medi-Cal patients for adverse childhood experiences (ACEs), in an effort California hopes will help prevent ongoing ACEs-related stress and disease,” according to a Salud America! report.
But it didn’t happen overnight. How did they get there?
To support statewide screening for ACEs, California:
- established an advisory group to provide recommendations regarding screening for ACEs
- allocated funding to support routine screening for ACEs
- launched an initiative to train providers on screening for ACEs and on recognizing and responding to toxic stress
- created methods for continuous quality improvement
The following sections explore each step in the process.
California’s Response: Support Statewide Screening for ACEs, Starting with an Advisory Group
In 2017, the California General Assembly passed a bill establishing a Trauma Screening Advisory Group to provide recommendations on specific trauma screening tools which could be utilized by the state’s Medicaid program, Medi-Cal.
State legislation is an important aspect of building a legal framework from which to address ACEs and toxic stress and is gaining momentum across the country.
In 2018, five legislative proposals in three states were adopted that incorporated ACEs. In 2019, eight legislative proposals in five states were adopted, according to the Injury Prevention Legislation Database of the National Conference of State Legislatures.
California’s Trauma Screening Advisory Group submitted its recommendations in January 2019, recommending that Medi-Cal providers screen for ACEs.In March 2019, the California Department of Health Care Services (DHCS) selected the Pediatric ACEs and Related Life-Events Screener (PEARLS) tool for children and the ACE Assessment for adults.
California’s Response: Support Statewide Screening for ACEs, with Allocation of Funding
Over two fiscal years (2019-2020 and 2020-2021), the state approved $143.1 million to support routine ACE screening primary care through Medi-Cal.
This included $78.4 million to train providers and $64.7 million to reimburse providers.
This budget supported the conceptual framework Burke Harris and her team created to train providers on screening for ACEs and on recognizing and responding to toxic stress and to reimburse trained providers to screen for ACEs in primary care and other specified settings.
California’s Response: Support Statewide Screening for ACEs, by Launching the ACEs Aware Initiative
With the funding provided, California launched the ACEs Aware initiative.
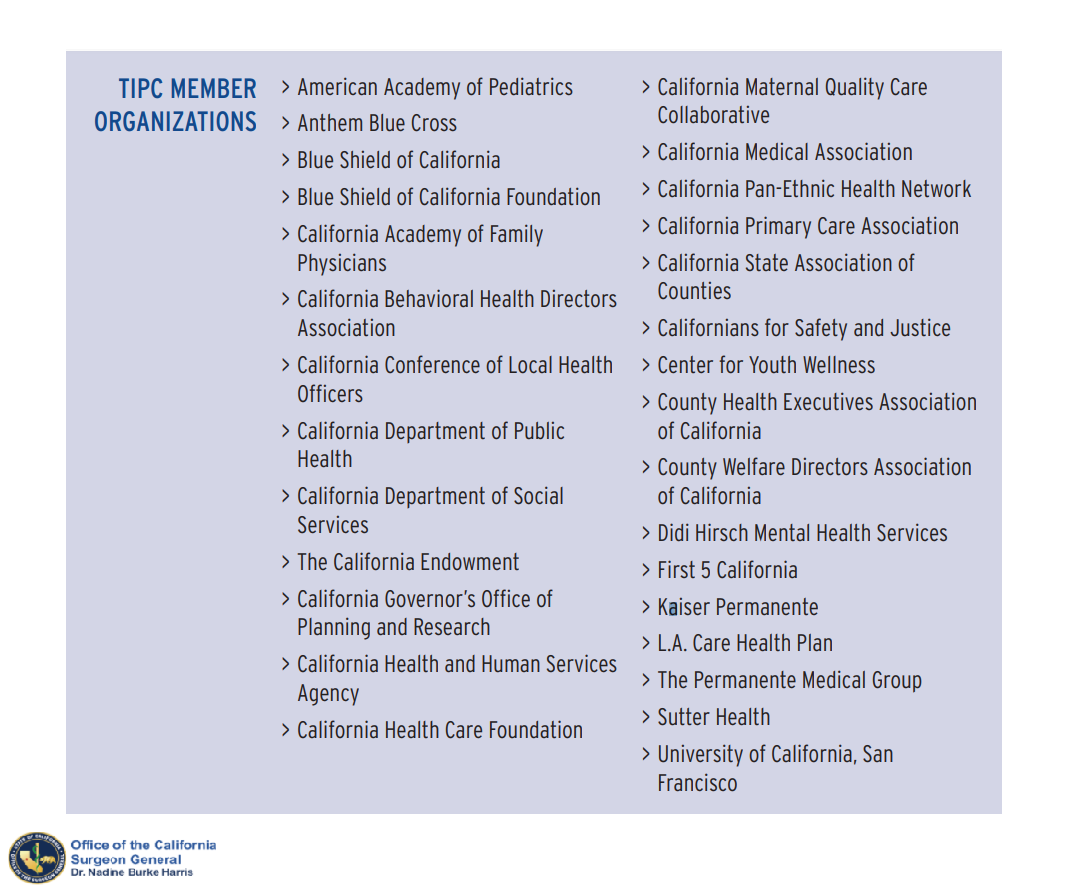
ACEs Aware is advised by the Trauma-Informed Primary Care Implementation Advisory Committee (TIPC) on promising models, best practices, evolving science, clinical expertise, and strategy for the implementation of trauma-informed care systems in California.
This novel clinical and public health effort utilizes training and key partnerships to build clinical and cross-sector capacity and empower Medi-Cal primary care providers to improve health outcomes by advancing the quality and efficiency of care provided to individuals exposed to ACEs or at risk for toxic stress.
“ACEs Aware seeks to accelerate adoption and spread of best practices to advance successful prevention, screening, and treatment for the impacts of ACEs and toxic stress in the healthcare setting,” Burke Harris’ report states.
They started by developing a two-hour, online training for primary care providers. The California Surgeon General’s Clinical Advisory Subcommittee (CAS)─composed of medical, behavioral health, and public health experts─developed the training by adapting and adding evidence-based content to a case-based curriculum originally developed by the Office of Women’s Health of the United States Department of Health and Human Services.
The Becoming ACEs Aware in California training includes 11 common pediatric and adult primary care case studies with free Continuing Medical Education (CME) and Maintenance of Certification (MOC) credits. Beginning December 2019, this training was offered for free.
In the first nine months, nearly 14,000 healthcare providers completed the training.
“Training primary care providers enables early detection of toxic stress, at a time when interventions are less intensive, less expensive, and more likely to be effective,” Burke Harris’s report states. “This allows providers to diagnose and treat patients based on an evidence-based assessment of risk—rather than waiting for patients to manifest the health, mental health, and behavioral consequences of toxic stress, when they are more difficult and more expensive to treat.”
ACEs Aware has also hosted monthly webinars featuring clinicians who share practical information.
Moreover, ACEs Aware is coordinating with managed care plans to ensure that they are encouraging and implementing ACE screening and response among Medi-Cal providers.
“Objectives include ensuring that MCPs and delegated entities understand how to implement and oversee ACE screening, billing, and payment; have the resources and tools to support primary care providers and teams; and develop the internal infrastructure to support primary care providers in implementing ACE screening and response,” Burke Harris’ roadmap states.
Beyond providing payment, training, and implementation support, ACEs Aware focuses on systems-level changes and “top-down” policies to strengthen provider engagement and capacity.
To support systems-level changes:
- ACEs Aware developed screening workflows and toxic stress risk assessment and response algorithms for both pediatric and adult care.
- ACEs Aware awarded $14.3 million in grants to 100 organizations in the areas of provider engagement, training, and communications, to deepen engagement and encourage the proliferation and sharing of best practices and strategies.
- ACEs Aware is creating a Network of Care Roadmap to improve collaboration and coordination across the healthcare and cross-sector systems to address toxic stress.
Supportive “top-down” policies include:
- Performance metrics and performance feedback to drive continuous QI in prevention, identification and response to ACEs, toxic stress, and ACE-Associated Health Conditions (AAHC)
- Programs to identify and financially reward providers and clinics that are meeting or exceeding performance metrics to incentivize high quality of care for ACEs, toxic stress, and AAHCs
- Effective use of the electronic medical record (EMR) to streamline care for ACEs, toxic stress, and AAHCs
Among the 100 grants provided, for example, some helped educate Medi-Cal providers on using ACE screening; support providers and other stakeholders in sharing lessons learned and best practices that are tailored to specific geographic areas, patient populations, provider types, and practice settings; and support strategic communications efforts and to promote the work of fellow grantees.
To support and develop consistent and effective messaging on ACEs and toxic stress, ACEs Aware engaged the Frameworks Institute, an internationally renowned organization with experience in using the science of framing to develop effective communication to spark change.
“A systems-level approach is required to consider and facilitate enhanced models of care, payment models for preventive visits, acute hospital and emergency room visits, and resources for individuals with emergent and/or chronic conditions,” Burke Harris’s report states.
In December 2020, ACEs Aware announced a second round of grants of up to $30 million to support Medi-Cal providers and their communities in effectively responding to ACEs.
The state recognizes there are still issues to address, such as:
- Clinicians are limited by current diagnostic codes, which do not include toxic stress physiology, thus may inhibit efforts to provide-trauma informed and healing-centered interventions.
- Through the Affordable Care Act, California chose to cover all essential health benefits, resulting in a substantial expansion of behavioral health services; however, there remains a shortage of behavioral healthcare workers.
- There is a need to integrate primary care and behavioral health within the same setting.
- Robust data-sharing systems are needed to avoid multiple efforts to screen the same patient and to advance scientific investigation of ACEs, toxic stress, and AAHCs.
“Shifts in diagnostic and billing codes for AAHCs and different clinical risk levels for toxic stress, combined with enhanced payment models to support brief interventions, care coordination, referrals, and frequency of follow-up, will enable more effective and coordinated action to prevent and heal the impacts of ACEs,” Burke Harris report states.
California’s Response: Support Statewide Screening for ACEs, including Enabling Quality Improvement
Quality improvement methods and tools are important to identify and develop innovations on a small scale as well as implementation and learning to scale up and spread across systems.
California created an 18-month public-private learning collaborative of 53 clinics in seven diverse California regions to assess best practices and inform implementation of future phases of the ACEs Aware initiative.
California ACEs Learning and Quality Improvement Collaborative (CALQIC) was created as a collaboration between by the University of California, San Francisco (UCSF), CA-OSG, and DHCS.
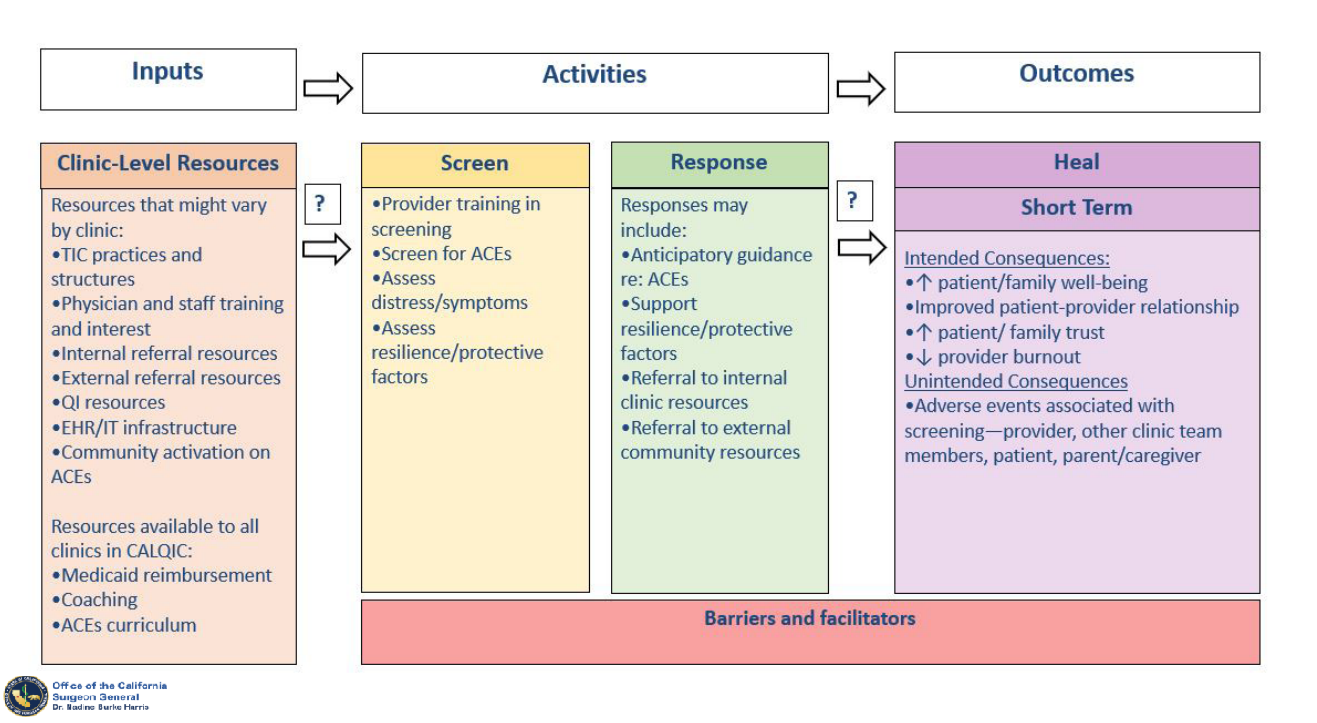
CALQIC supports participating clinics to:
- Identify and overcome barriers to ACEs screening and response at both the site and organizational levels
- Develop or strengthen models of care and tools for operationalizing ACEs screening and response (i.e., clinical roles, workflows, and scripts)
- Align clinical efforts with the statewide initiative, ACEs Aware, which is working to ensure providers are credentialed, use approved screening tools, and bill using appropriate codes
- Advance health equity
- Collect and track data to assess progress in ACEs screening and response
- Identify and respond to any potential adverse events associated with ACE screening
“Ultimately, the lessons learned in CALQIC will inform best practices in ACE screening and response, help avoid unintended harms, and guide future implementation efforts in other clinics and health systems throughout California and nationally,” Burke Harris’ report states.
The state also compiled seven case studies of current successful clinical implementation of ACE screening and response to enhance local learning regarding innovations, opportunities, and challenges.
“As clinical sites work to integrate approaches to mitigating ACEs and toxic stress, current successful clinical implementation efforts of early adopters provide key
insights and can help promote the diffusion of this innovative approach,” Burke Harris’ roadmap states.
California’s Response: Cross-Sector Coordination Within and Outside State Government, with Budgetary Support
California’s efforts also go well beyond ACEs screening.
Central to the state’s approach to reducing ACEs and toxic stress is a coordinated response system that involves a cross-sector budgetary approach and evidence-based strategies across all sectors of society throughout the state.
Cross-sector public health prevention strategies include intervening early, supporting parents and caregivers, creating stable and supportive early living conditions, reducing child poverty and economic insecurity, and ensuring high-quality child care.
Healthcare, public health, social services, early childhood, education, and justice sectors can all contribute to each level of public health prevention.
“Resources and services could include linkages to economic supports, legal supports (including medical-legal partnerships), high-quality evidence-based home visitation services, child care, preschool and school enrichment with family engagement, and parenting or family relational skill-building,” Burke Harris’ report states.
Burke Harris convened the following two important groups of leaders within and outside state government to educate about the impacts of ACEs, coordinate existing efforts, and advise on best practices:
- An ACEs Reduction Leadership Team with directors of key departments in the Health and Human Services Agency, the California Department of Corrections and Rehabilitation, the California Department of Education, and the Governor’s Office, among others
- The Trauma-Informed Primary Care Implementation Advisory Committee (TIPC), which is composed of representatives of major healthcare plans, health systems, philanthropic associations, nonprofits, local government associations, professional provider associations, and subject matter experts
“California has made several key budget investments in cross-sector work that have strengthened supports for children and families, helped them become more resilient, and prevented the incidence and intergenerational transmission of ACEs and toxic stress,” Burke Harris’ report states.

For example:
- To strengthen economic supports for families, California increased the Maximum Aid Payment available through the CalWORKs program, a public assistance program that provides cash aid for housing, food, utilities, clothing, or medical services to eligible families with children, including families with caregiver absence, death, or disability.
- To strengthen economic supports for families, California has continued to expand the reach of its Paid Family Leave Program, which provides economic support to eligible working families through partial wage replacement benefits.
- To strengthen early learning and care, California created the Master Plan for Early Learning and Care, which is a long-term strategic plan to provide a series of reports to inform the advancement of comprehensive, high-quality, and affordable child care and preschool for children from birth through age 12 years.
- To strengthen early learning and care, California convened the Early Childhood Policy Council to provide recommendations to the legislature and the administration on state early learning and care policy.
- To expand healthcare coverage, under the Affordable Care Act, California has further expanded Medi-Cal by expanding the duration of coverage for eligible pregnant women diagnosed with a maternal mental health condition and expanding full-scope Medi-Cal coverage to undocumented young adults age 19 through 25.
- To advance research and biomedicine, the California Initiative to Advance Precision Medicine issued an request for proposals to provide $9 million in grants to support precision medicine approaches to advance the assessment and treatment of ACEs and toxic stress.
“Appropriately recognizing toxic stress as a health condition allows all sectors to understand and frame its consequences through that lens,” Burke Harris’ report states. “This allows for the adoption of aligned legal, policy, and regulatory frameworks in response.”
California’s Response: Cross-Sector Coordination Within and Outside State Government, with Evidence-Based Strategies
Improving social and health outcomes requires a wide array of community-based city, county, and regional efforts.
Burke Harris’s roadmap includes prevention strategies in healthcare, public health, social services, early childhood supports, education, and justice that foster a shared vision for well-being and healing, with sustainable cross-agency and cross-sector collaboration.
For example, two counties in California are implementing the Handle With Care initiative, which notifies schools when children are present at the scene of an encounter with law enforcement so that schools are prepared to respond proactively by handling that student with care.
We cover each of the sectors in detail in our 11-part series.
Evidence-based staff interventions, support coaching, and practicing compassionate resilience are important to support workers across sectors and prevent fatigue, burnout, vicarious trauma, and turnover.
“Trauma-informed, toxic-stress-responsive training enables all front-line providers, such as educators and law enforcement officers, to recognize the symptoms of a dysregulated stress response due to toxic stress so that they can respond with trauma-informed, evidence-based principles, rather than escalate the encounter, for instance, through harsh punitive measures.” Burke Harris’ roadmap states.
However, there is a need to standardize language, definitions, and guidelines across these cross-sector trainings.
California also recognizes the need support trauma-informed, patient-center medical homes.
“The capacity for a medical home to become a trauma-informed, multidisciplinary system is a foundational building block of this initiative,” Burke Harris’ report states.
This can be achieved by:
- funding and incentives for best practices
- creating, disseminating, and coordinating efforts to expand this model across federally qualified health centers in California
- creating performance measurement standards and requirements
- offering free provider trainings with Continuing Medical Education (CME) and Maintenance of Certification (MOC) credit
- supporting quality improvement efforts
Additionally, care coordinators, health educators, and patient navigators play an important role in connecting families to appropriately targeted services and resources, such as economic supports, legal supports, high-quality evidence-based home visitation services, child care, and preschool.
Policies that allow for the credentialing and/or compensation for these workers can strengthen closed-loop referral systems and further support cross-sector coordination.
California’s Response: Assess Best Practices in Trauma-Informed Care Across the State
Because numerous state agencies and organizations already initiate and collaborate on efforts to improve social and health outcomes, it is important to better understand what baseline efforts are already underway to make California a more trauma-informed state.
In coordination with the California Department of Public Health, the Strategic Growth Council, and DHCS, Burke Harris has implemented two environmental scans to assess the status of current State and County efforts to prevent and address ACEs and toxic stress across all sectors, and to identify opportunities for future expansion and collaborations.
The state surveyed county and state leaders in public health, education, early childhood, home visitation, justice, and social services about the reach and extent of their organization’s work related to ACEs. Survey questions were informed by ACEs Connection’s Milestone Tracker.
The survey aimed to develop a baseline understanding of:
- the current level of awareness of ACEs
- the current level of training and education efforts around ACEs
- adoption of ACEs-related and trauma-informed policies and practices
- implementation of ACEs-related and trauma-informed policies and practices
With a better understanding of existing supports and challenges, the state can promote promising practices and target support where needed.
“The results of the surveys are intended to inform the cross-sector strategies, including of the ACEs Aware and [Essentials for Childhood (EfC)] initiatives, around state- and local-level efforts to incorporate trauma-informed approaches into their systems and ultimately reduce ACEs,” Burke Harris’ roadmap states.
State officials emailed state surveys directly to 400 individuals from 50 state departments using both a broad outreach that relied on formal state organizational structure and a targeted outreach that relied on personal connections among the survey team. In total, 261 individuals at 32 state departments responded.
Similarly, state officials emailed the county survey directly to 550 individuals from 58 county organizations using both broad and targeted outreach. In total, 257 individuals serving 57 of the 58 counties in California responded.
Survey results are expected to be released in spring 2021.
“These reports will include a summary of the results of the two surveys, as well as recommendations for state and local agencies and organizations regarding promising practices that can be used to make California a resilient and trauma-informed state, how to better meet the needs of the Californians who have faced adversity, and how to best support the staff who provide those services,” according to Burke Harris’ roadmap.
What Can We Do About Toxic Stress?
Share our Salud America! team’s 11-part exploration into the important recommendations in Dr. Nadine Burke Harris’ roadmap to address ACEs and toxic stress:
- Toxic Stress and its Lifelong Health Consequences. Toxic stress is a public health crisis that has lifelong impacts on physical, mental, and behavioral health.
- We Need to Recognize Toxic Stress as a Health Condition with Clinical Implications. Health experts are pushing to elevate toxic stress and developmental trauma on national research and policy agendas.
- Cut Toxic Stress with 3 Types of Public Health Prevention Interventions. Preventing toxic stress requires a three-level public health intervention approach.
- How to Use Healthcare Strategies to Address Toxic Stress. In clinics, hospitals, and other healthcare settings, workers can provide universal trauma-informed care and more.
- Using Public Health Strategies to Address Toxic Stress. When it comes to ACEs and resulting toxic stress, the public health sector can play a critical role by strengthening economic support, positive family relationships, and social services.
- How to Use Social Service Strategies to Address Toxic Stress. We need trauma-informed training for social workers, as well as family-friendly workplaces and home visits.
- Toxic Stress in Early Childhood and How to Prevent It. Early childhood is a key time for preventing ACEs and toxic stress.
- Toxic Stress in Justice and How to Address It. Encounters with police are “intrinsically stressful and potentially traumatic,” especially for youth of color.
- Toxic Stress in Education and How to Address It. ACEs and toxic stress can hinder a person’s learning and school success.
- California’s Epic Response to Toxic Stress and ACEs. California, already leading the nation in addressing ACEs, is making inroads to address toxic stress. (current article)
- 5 Upstream Ways You Can Take Action to Address Toxic Stress. Here are ways you can take action to address toxic stress.
“Increasing the familiarity of clinicians and researchers with ACEs and toxic stress can serve to enlist greater numbers of scientific professionals to develop more effective science-based treatments and interventions for toxic stress and to rigorously evaluate their efficacy, thereby directly advancing the science and clinical management of ACEs and toxic stress,” Burke Harris’ roadmap states.
By The Numbers
142
Percent
Expected rise in Latino cancer cases in coming years



