Share On Social!
Toxic stress is endangering the current and future health of our society.
Amid the mental, physical, and economic toll of the COVID-19 pandemic, there is even greater need to prevent the risk factors for toxic stress, which are severe, intense, or prolonged stress, trauma, or adverse childhood experiences (ACEs) like physical, sexual, and emotional abuse.
The new Roadmap for Resilience: The California Surgeon General’s Report on Adverse Childhood Experiences, Toxic Stress, and Health is the nation’s first guide to address toxic stress by cutting ACEs in half in a generation.
We at Salud America! are exploring the roadmap in an 11-part series.
This is the final post in the series, with five upstream ways you can take action to address toxic stress.
“To enable lasting change, healthcare-based innovations must be closely coordinated with cross-sector response, practice transformation, research and innovation, and public education efforts,” according to the roadmap, led by Nadine Burke Harris.
1. Spread the Word about ACEs and Toxic Stress
It is important to raise awareness about social problems and evidence-based solutions to garner public and political will for necessary policy and systems changes.
Because ACEs are a national problem, we need public education campaigns to enhance understanding and shift public discourse and social norms away from blaming individuals and towards solutions to address upstream, systemic causes of stress in communities.
We need a public education campaign that:
- Explains how ACEs and toxic stress impact well-being;
- Focuses on the structural and systemic conditions that can make ACEs and toxic stress more or less likely to occur; and
- Features strong messages of hope, including practical strategies for scaffolding protective factors and how to break the intergenerational cycle of adversity.
“Policy- and systems-level efforts to prevent ACEs and toxic stress also depend on the awareness and engagement of the general public and governmental decision-makers,” according to Burke Harris’ roadmap. “The ‘political will’ to implement pro-child, pro-family policies and budgets is influenced by social norms about the status of children and the loci of responsibility for their well-being.”
However, to deliver messages to raise awareness and shift social norms, you have to know what to emphasize, what to leave unsaid, and how to explain complex concepts.
That’s why the FrameWorks Institute created a communications toolkit for talking about toxic stress with general guidelines and evidence-based best practices.
“The strategies in this ToolKit are designed to help advocates, pediatricians, direct service providers, and other frontline professionals to more effectively communicate the science of development with members of communities dealing disproportionately with economic and socio-cultural disadvantage,” according to the FrameWorks toolkit.
For example, the toolkit includes strategies for effectively communicating about toxic stress with the following five framing recommendations:
- Don’t talk about toxic stress without also explaining people’s capacity for resilience.
- Place parenting in context to reduce stigma and guilt.
- Emphasize self-efficacy rather than Individualism.
- Build understanding that toxic stress is a public concern in need of community-based solutions.
- Don’t rely on the value of science alone.
Instead of stating that children who experience early adversity will have more health problems later in life, try explaining that over time and without supports, children who experience early adversity are more likely to have health problems later in life.
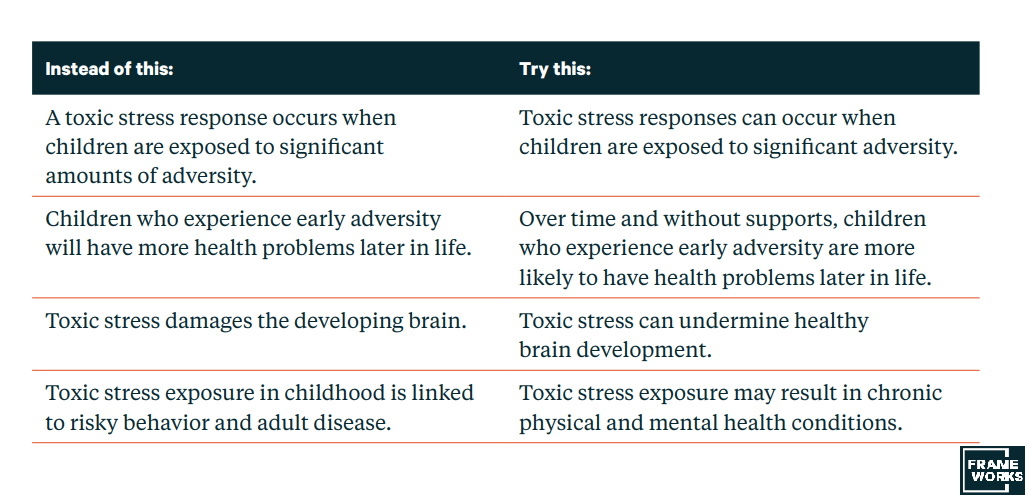
It is also important to emphasize the importance of community-based solutions to build community strength and resilience.
Additionally, instead of citing non-specific “experts” to establish authority on a subject, which can feed skepticism and cynicism, try being as specific and concrete as possible when referring to research and appeal to the value of ingenuity to emphasize how science can be used to solved problems.
“Strategic framing is about knowing both what to say and what not to say to help people reason productively about a topic,” according to FrameWorks.
Public education campaigns are also important to bolster interventions and skills individuals can learn to regulate their stress responses, including improving:
- Sleep
- Nutrition
- Physical activity
- Healthy relationships
- Access to nature
- Mindfulness practices
- Mental healthcare
“Past public education campaigns have been effective at reducing the prevalence of health conditions and risk factors, including smoking, lead poisoning, and motor vehicle deaths,” according to Burke Harris’ roadmap.
These campaigns are most effective when partnered with concrete policy efforts informed by a public health approach.
2. Prioritize a Public Health Approach to Prevent Toxic Stress
To reduce the impact of disease, public health leaders usually apply a three-part preventive approach of prevention, early detection, and early intervention.
For example, to prevent diabetes, HIV, and COVID-19, and lessen the consequences of these diseases, public health leaders use this three-part approach:
- Primary prevention includes efforts that target healthy individuals and aim to prevent harmful exposures and behaviors from ever occurring.
- Early detection, also known as secondary prevention, involves screening to identify risk factors and/or diseases in the earliest stages, before the onset of signs and symptoms.
- Early intervention or treatment, also known as tertiary prevention, includes efforts that target individuals who have already developed a disease or social outcome to lessen the severity, progression, or complications associated with the disease or social outcome.
Primary prevention strategies are particularly important to change structural and systemic conditions to prevent unhealthy behaviors and risk factors, and increase healthy behaviors and protective factors.
These are known as upstream strategies because they have the potential to impact entire populations and require less individual effort.
Now, a similar approach is needed to prevent ACEs and toxic stress.
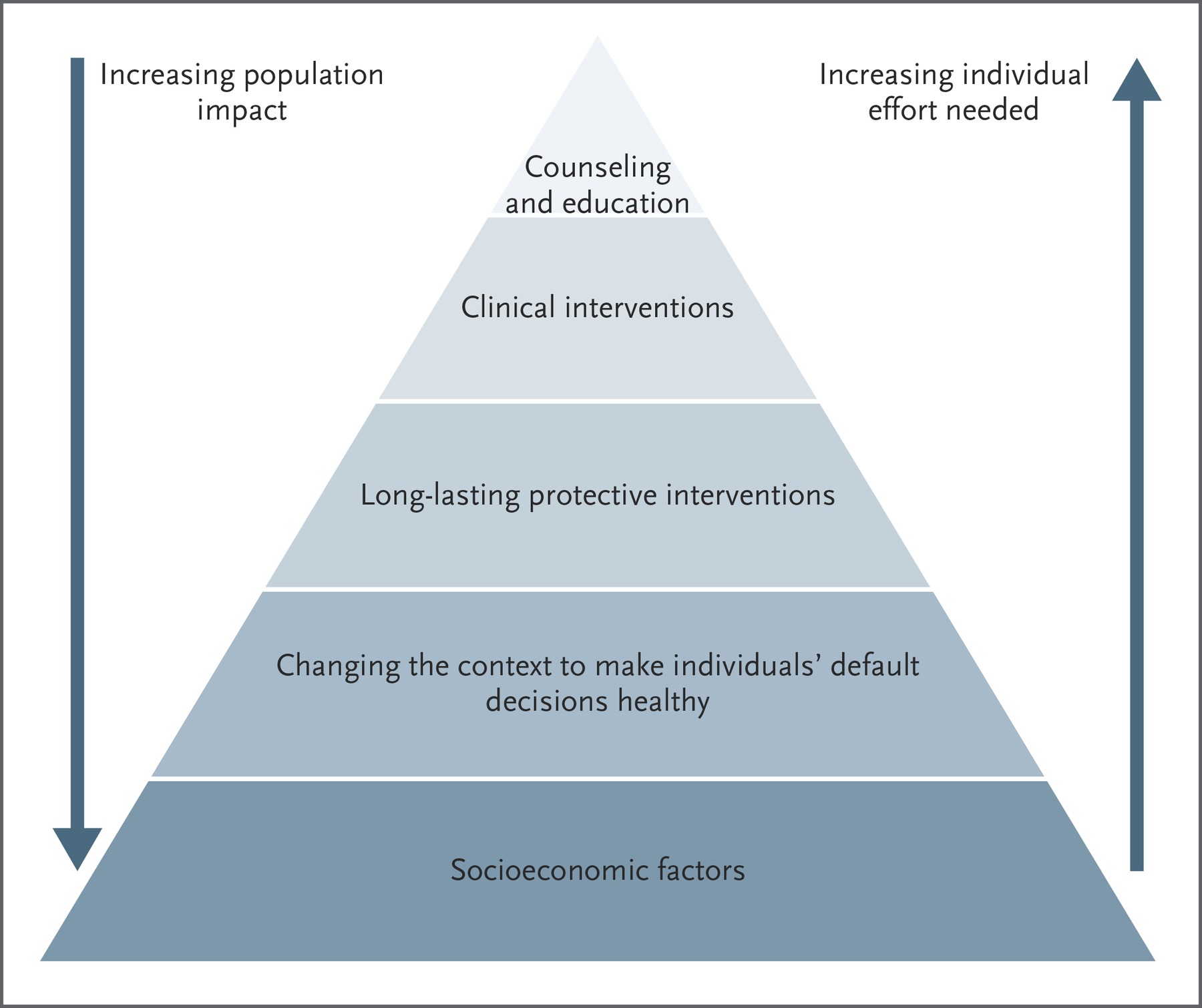
After all, toxic stress is a health condition with clinical implications.
That’s why Burke Harris’ new roadmap provides prevention, early detection, and early intervention strategies for policymakers, scientists, healthcare providers, educators, and advocates to prevent toxic stress and address trauma.
To enable lasting change, we need to be familiar with three-part preventive approach strategies across healthcare, public health, social services, early childhood supports, education, and justice, and we need to foster cross-sector collaborations to implement effective intervention and prevention tactics.
“The state of California has set a bold goal to cut the burden of toxic stress and ACEs in half in the next generation by implementing a well-formulated public health approach to prevention, early detection, treatment and cross-sectoral action,” according Burke Harris’ roadmap. “To do this, California is addressing upstream factors, supporting family and community resilience, and prioritizing equity in achieving health and social outcomes.”
3. Push for Trauma-Informed Care across Your County and State
In communities across the country, multiple sectors are collaborating to address ACEs and toxic stress by working toward becoming trauma-informed.
For example:
- In this Texas city, leaders got together to launch a trauma-informed consortium and created the city’s first-ever position dedicated to supporting the consortiums work to create a network of coordinated trauma-informed care for children and families facing adversity.
- A national organization in New Jersey worked with police to explore trauma and build community trust.
- In this Oregon city, a superintendent started a mental health services in his district and pushed to start a statewide learning collaborative to educate other school districts on how to support students who face trauma.
- School leaders in Nevada partnered with police to launch the Handle With Careinitiative, which notifies schools when children are present at the scene of an encounter with law enforcement, so that schools are prepared to respond proactively by handling that student with care.

Because many groups are already working together to improve social and health outcomes, it is important to better understand what baseline efforts are already underway in your community and state.
That’s why leaders in California implemented two environmental scans to assess the status of current State and County efforts to prevent and address ACEs and toxic stress across all sectors. This also helped identify opportunities for future expansion and collaborations.
The state surveyed county and state leaders in public health, education, early childhood, home visitation, justice, and social services about the reach and extent of their organization’s work related to ACEs. Survey questions were informed by ACEs Connection’s Milestone Tracker.
The survey aimed to develop a baseline understanding of:
- the current level of awareness of ACEs
- the current level of training and education efforts around ACEs
- adoption of ACEs-related and trauma-informed policies and practices
- implementation of ACEs-related and trauma-informed policies and practices
With a better understanding of existing supports and challenges, the state can promote promising practices and target support where needed.
Survey results are expected to be released in spring 2021.
“These reports will include a summary of the results of the two surveys, as well as recommendations for state and local agencies and organizations regarding promising practices that can be used to make California a resilient and trauma-informed state, how to better meet the needs of the Californians who have faced adversity, and how to best support the staff who provide those services,” according to Burke Harris’ roadmap.
4. Push for Statewide Screening for ACEs
As a secondary public health prevention strategy, the goal in screening for ACEs is to target interventions to those who need them most early, when interventions are likely to be more effective and less expensive.
Screening, however, requires evidence-based biomarkers to test and diagnostic criteria to determine to what is or isn’t normal function.
Unfortunately, there are no nationally agreed-upon biomarkers, tests, or diagnostic criteria for toxic stress.
 While some potential biomarkers have been proposed─such as markers of inflammation, stress, altered metabolism, cellular aging, and epigenetic regulation─more research is needed to validate and translate biomarkers for use in clinical diagnosis and treatment.
While some potential biomarkers have been proposed─such as markers of inflammation, stress, altered metabolism, cellular aging, and epigenetic regulation─more research is needed to validate and translate biomarkers for use in clinical diagnosis and treatment.
In the meantime, California is taking action.
California is relying on the Pediatric ACEs and Related Life-events Screener (PEARLS) test for healthcare providers to assess children for the 10 original categories of ACEs—as well as seven additional categories of trauma.
In 2017, the California Legislature passed Assembly Bill 340 (AB340), which calls for a trauma screening advisory group to update, amend, or develop tools and protocols for screening children for trauma within the Early and Periodic Screening, Diagnosis, and Treatment (EPSDT) Medicaid benefit.
The goal of the EPSDT benefit is to ensure children younger than 21 who are enrolled in Medicaid get age-appropriate screening, preventive services, and treatment services that are medically necessary to correct or ameliorate any identified conditions.
In January 2019, the advisory group submitted its recommendations to the California Department of Health Care Services (DHCS) and the Legislature
Based on those recommendations, DHCS proposed that Medi-Cal primary care providers use the PEARLS Tool.
Developed by the Bay Area Research Consortium on Toxic Stress and Health, PEARLs scores include two numbers: one for the traditional ACE score which ranges from 0 to 10; and one for the additional section which ranges from 0 to 7.
For example, diagnostic criteria for characterizing patient’s risk of manifesting a toxic stress response based on the traditional 10 ACE categories includes:
- A score of 0 indicates low risk
- A score of 1-3 without associated health conditions indicates intermediate risk
- A score of 1-3 with associated health conditions indicates high risk
- A score of 4+ with or without associated health conditions indicates high risk.
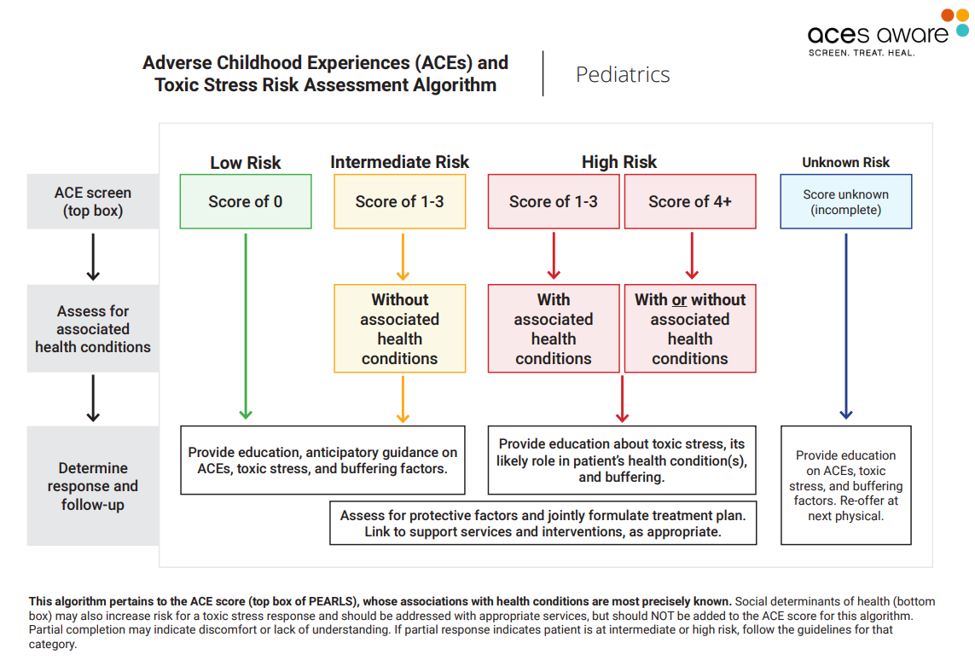
Physicians then use a screening/scoring algorithm to identify children facing low-, intermediate- or high risks of symptoms and health problems associated with ACEs.
When a child is identified as high risk, with or without associated health conditions, the pediatrician will:
- Provide education about toxic stress, its likely role in the patient’s health condition(s), and buffering;
- Assess for protective factors and jointly formulate a treatment plan; and
- Link to support services and interventions, as appropriate.
Over the next two fiscal years (2019-2020 and 2020-2021), the state of California approved $143.1 million to support routine ACE screening through Medi-Cal.
This funding is intended to train primary care providers to conduct ACEs screening and to reimburse primary care providers for conducing ACEs screening.
To achieve this, the state launched an initiative to train providers on screening for ACEs and on recognizing and responding to toxic stress to include developing a two-hour, online training for primary care providers.
They also created methods for continuous quality improvement.
“Training primary care providers enables early detection of toxic stress, at a time when interventions are less intensive, less expensive, and more likely to be effective,” Burke Harris’s report states. “This allows providers to diagnose and treat patients based on an evidence-based assessment of risk—rather than waiting for patients to manifest the health, mental health, and behavioral consequences of toxic stress, when they are more difficult and more expensive to treat.”
5. Push for National Toxic Stress Research and Policy Agendas
As mentioned previously, more research is needed to establish clinical diagnostic criteria for toxic stress.
To advance a robust toxic stress research agenda, key objectives include:
- Development of clinically relevant biomarkers to help more precisely diagnose, classify, and assess treatment efficacy for toxic stress in clinical settings.
- Guidelines for clinical management of ACE-Associated Health Conditions (AAHCs) in the setting of toxic stress.
- Identification of therapeutic targets for regulating the toxic stress response.
- Elucidation of the complex interactions of how individual differences in underlying biological susceptibility or exposures might affect clinical presentation of toxic stress or inform individualized treatment strategies.
- Longitudinal studies to better understand the specific and longer-term impacts of clinical interventions that target the toxic stress response, especially for metrics like prevalence and severity of AAHCs, social outcomes, healthcare utilization, systems-level costs, and health equity. Tracking and preventing unanticipated harms will be of paramount importance.
“Development of clinical diagnostic criteria for toxic stress is a key milestone that has the potential to greatly improve quality, efficacy, and coordination of care, and reimbursement for services,” according to Burke Harris’ roadmap.
The following biomarkers have been associated with toxic stress and/or ACEs, according to Burke Harris’ roadmap:
- Markers of inflammation, such as soluble urokinase plasminogen activator receptor (suPAR), interleukin-6 (IL-6) and tumor necrosis factor-alpha (TNF-α), and C-reactive protein (CRP).
- Markers of stress and stress reactivity, such as cortisol: both higher and lower levels of cortisol have been reported in toxic stress.
- Markers of altered metabolism, such as leptin; ghrelin; neuropeptide-Y (NPY); and mitochondrial DNA accumulation.
- Marker of cellular aging, such as telomere length.
- Markers of epigenetic regulation, such as various, including methylation of the serotonin promoter and FκBP5.
“These biomarkers and the clinical pathways they inform may also offer insight into potential therapeutic targets and precision medicine treatments to ameliorate the impact of toxic stress on health and well-being,” according to Burke Harris’ roadmap.
Some think that including toxics stress in the International Classification of Diseases-Clinical Modification, Tenth Revision (ICD-10-CM) will better support research and development of diagnostic criteria as well as translation into practice.
Research is critical to inform policy.
Groups like Gravity Project and the Campaign for Trauma-Informed Policy and Practice (CTIPP) are pushing for a research-based policy agenda.
The Gravity Project is a coalition of experts working towards consensus-driven standards on social determinants of health. They recently proposed social risk codes to CDC National Center for Health Statistics’ ICD-10-CM, and they currently have a committee dedicated to discussing stress.
CTIPP, is a group of experts from diverse sectors who volunteer to work in collaboration with government, organizations and citizens to develop trauma-informed, prevention-focused, evidence-informed policies and practices that promote a comprehensive, integrated multi-sector approach for building trauma-informed communities.
In January, 2021, they released a policy brief suggesting a trauma-informed agenda for the first 100 days of the Biden-Harris Administration. The policy brief provides short-term priorities to address the psycho-social-emotional impact of the pandemic, as well as short-term priorities to address ACEs and toxic stress.
Priorities include establishing a goal of preventing ACEs and reducing their impact by 50% by 2030, as well as:
- Secondary and vicarious trauma: Recipients of funds in any new stimulus bill should be advised on how they can use those funds to provide trauma-informed and resilience strategies for those most at-risk for secondary/vicarious trauma, such as teachers, law enforcement officers, first responders, nurses and other healthcare workers, mental health and social welfare workers and others serving people and communities affected by the pandemic.
- Racial, intergenerational, and historical trauma: Increase representation of marginalized communities in shaping public policy and engage them in translating policy in local community action, particularly Latino and other communities of color, indigenous communities, LGBTQIA+ communities, and others have suffered throughout the history of our country.
- National healing campaign: Move the Interagency Task Force on Trauma-Informed Care from HHS to the White House and expand its responsibilities to develop a comprehensive plan to reach this goal of reducing ACEs by 2030. Prioritize approaches to serve marginalized communities suffering high levels of ACEs, diseases of despair, and associated health conditions
- Federal trauma-informed and anti-racism training: Require online trauma-informed and anti-racism trainings for all federal employees engaged in human services programs, with extra emphasis on reaching those in policy making positions.
- Addressing trauma at the border: Reallocate funds from the Border Wall and use it to provide trauma-informed services to promote healing among the families who suffer trauma as a result of family separation and other Border policies.
Numerous other national advocates are speaking up for a national policy agenda.
In July 2019, Dr. Christina Bethell with the Department of Population, Family and Reproductive Health at Johns Hopkins Bloomberg School of Public Health, testified to Congress about childhood trauma as pervasive public health issue that needs greater federal attention.
In January 2021, the International Transformational Resilience Coalition (ITRC) released the ITRC Mental Wellness and Resilience Policy calling for a public health prevention approach to preventing and healing toxic stress generated by the climate emergency.
The ITRC policy calls on Congress to enact and fund the Mental Wellness and Resilience Act (MWRA) to make the prevention of mental health and psychosocial problems a national priority and calls on the establishment of an Office of Mental Wellness and Resilience in the Department of Health and Human Services.
Untreated ACEs and toxic stress are the root cause of the most common and costly health conditions and they exacerbate inequities in social, economic, and health outcomes for generations to come.
Untreated ACEs and toxic stress represent an underaddressed public health crisis of our era.
“The time to act on this crisis is now,” Burke Harris’ roadmap states.
Other Ways to Help Address Childhood Trauma
Share our Salud America! team’s 11-part exploration into the important recommendations in Dr. Nadine Burke Harris’ roadmap to address ACEs and toxic stress:
- Toxic Stress and its Lifelong Health Consequences. Toxic stress is a public health crisis that has lifelong impacts on physical, mental, and behavioral health.
- We Need to Recognize Toxic Stress as a Health Condition with Clinical Implications. Health experts are pushing to elevate toxic stress and developmental trauma on national research and policy agendas.
- Cut Toxic Stress with 3 Types of Public Health Prevention Interventions. Preventing toxic stress requires a three-level public health intervention approach.
- How to Use Healthcare Strategies to Address Toxic Stress. In clinics, hospitals, and other healthcare settings, workers can provide universal trauma-informed care and more.
- Using Public Health Strategies to Address Toxic Stress. When it comes to ACEs and resulting toxic stress, the public health sector can play a critical role by strengthening economic support, positive family relationships, and social services.
- How to Use Social Service Strategies to Address Toxic Stress. We need trauma-informed training for social workers, as well as family-friendly workplaces and home visits.
- Toxic Stress in Early Childhood and How to Prevent It. Early childhood is a key time for preventing ACEs and toxic stress.
- Toxic Stress in Justice and How to Address It. Encounters with police are “intrinsically stressful and potentially traumatic,” especially for youth of color.
- Toxic Stress in Education and How to Address It. ACEs and toxic stress can hinder a person’s learning and school success.
- California’s Epic Response to Toxic Stress and ACEs. California, already leading the nation in addressing ACEs, is making inroads to address toxic stress.
- 5 Upstream Ways You Can Take Action to Address Toxic Stress. Here are ways you can take action to address toxic stress. (current article)
Salud America! also has two action packs to help you take action in your community.
Download the Salud America! “Trauma Sensitive School Action Pack” is a free guide with coaching to help school personnel talk to decision-makers, build a support team, craft a system to identify and support traumatized students, and more!
Download the Salud America! “Handle With Care Action Pack.” The action pack helps police, school, and mental healthcare leaders start the Handle with Care program, in which police notify schools when they encounter children at a traumatic scene, so schools can provide support right away. They can virtually support kids if school is out for summer or closed due to a pandemic like COVID-19.
“We believe our Action Pack will unite police, schools, and mental health leaders to support traumatized students,” said Dr. Amelie Ramirez, director of Salud America! at UT Health San Antonio. “Even with virtual school, Handle With Care can enable traumatized students achieve academically and emotionally at their highest level, while helping prevent future risky behavior and chronic disease.”
By The Numbers
142
Percent
Expected rise in Latino cancer cases in coming years



