
Share On Social!
Exposure to domestic violence and other adverse childhood experiences (ACEs) can trigger the toxic stress response for a long time, disrupting brain and body development and contributing to some of the most serious health conditions facing our society.
Public health can help prevent, detect, and mitigate toxic stress.
That’s why Dr. Nadine Burke Harris’ recent Roadmap for Resilience: The California Surgeon General’s Report on Adverse Childhood Experiences, Toxic Stress, and Health calls on public health leaders to address ACEs and toxic stress among Latinos and all people.
“The public health field plays an important role in ensuring that communities have healthy environments that support healthy behaviors and reduce risk of harmful exposures,” Burke Harris’ roadmap states.
Salud America! is exploring this as part of its 11-part series on toxic stress.
What Does the Public Health Field Do?
The public health sector is different than the healthcare sector.
Public health focuses on health from the perspective of populations, while the healthcare sectors focuses on health from the perspective of individuals.
“The public health sector’s long-standing mission is to promote and protect the health and well-being of entire populations, to seek to prevent disease and injuries before they happen, and to mitigate health consequences once disease, injury, or disaster does strike,” Burke Harris’ roadmap states.
The public health approach has a four-step process:
- Define and monitor the problem
- Identify and seek to reduce risks and increase protective factors
- Develop and test further prevention strategies
- Assure widespread adoption of prevention strategies
Over the past year, these four steps have been used to define and monitor COVID-19; to identify risks for infection and illness from COVID-19; to test strategies to prevent infection and illness from COVID-19; and to implement strategies to prevent infection and illness from COVID-19. This response has been especially important for Latinos, who suffer disparate pandemic effects.
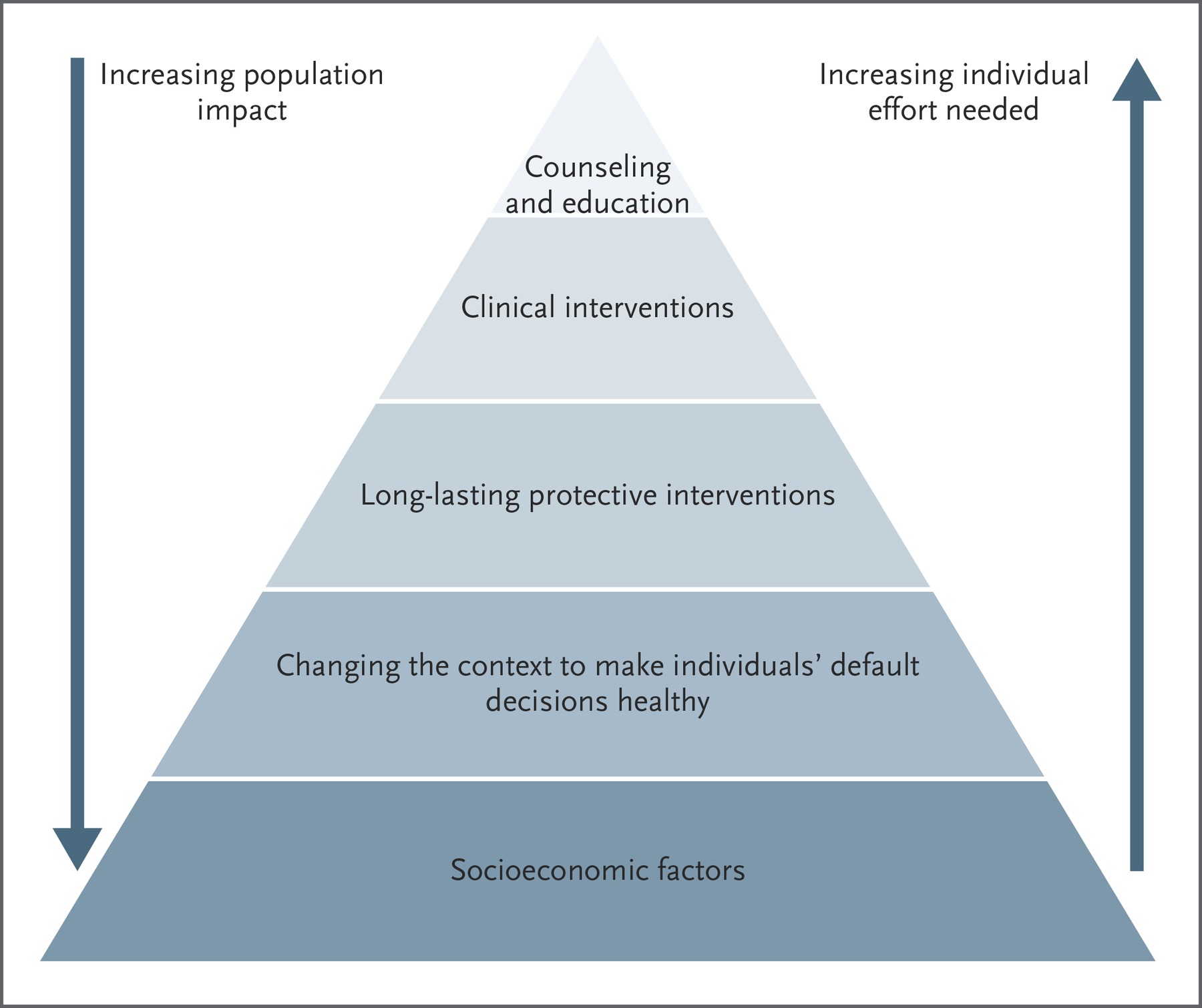
Public health has three types of prevention strategies:
- Primary prevention
- Secondary prevention or early detection
- Tertiary prevention or early intervention and treatment
Public health professionals work in national, state, and local governmental public health agencies. They also work with a wide range of academic, public, and private organizations.
They conduct surveillance and research, implement and evaluate population-level interventions, and advocate for public health solutions.
These interventions and solutions are often non-medical.
Instead, the public health field seeks to consider and address the conditions of daily life and the forces and systems that shape the conditions of daily life.
After all, health is shaped in large part by the policies and programs that inform land use planning, housing, transportation, and economic development.
Sadly, Latino communities face unaffordable housing, unreliable public transportation, and a lack of green space and parks, according to a Salud America! research review.
Additionally, many Latino families suffer a big lack of access to support for economic and educational success, according to another Salud America! research review.
“Multiple studies have shown that neighborhood characteristics (e.g., segregated and concentrated poverty) affect the level of violence, crime and delinquency, education performance, psychological distress, and various health problems,” Burke Harris’ roadmap states.
Systemic racism is another barrier.
“Institutional and personally mediated racism can result in trauma and chronic stress, as well as internalized racism and a diminished sense of self in youth of color,” Burke Harris’ roadmap states.
That’s why public health focuses on the social, environmental, economic, and political conditions that shape the places in which people are born, grow, work, live, and age.
Below are primary, secondary, and tertiary prevention strategies for the public health field to strengthen the capacity to mitigate the stress response and counteract the negative effects of ACEs.
Primary Prevention Strategies in Public Health
Primary prevention includes efforts that target healthy individuals and aim to prevent harmful exposures and behaviors from ever occurring.
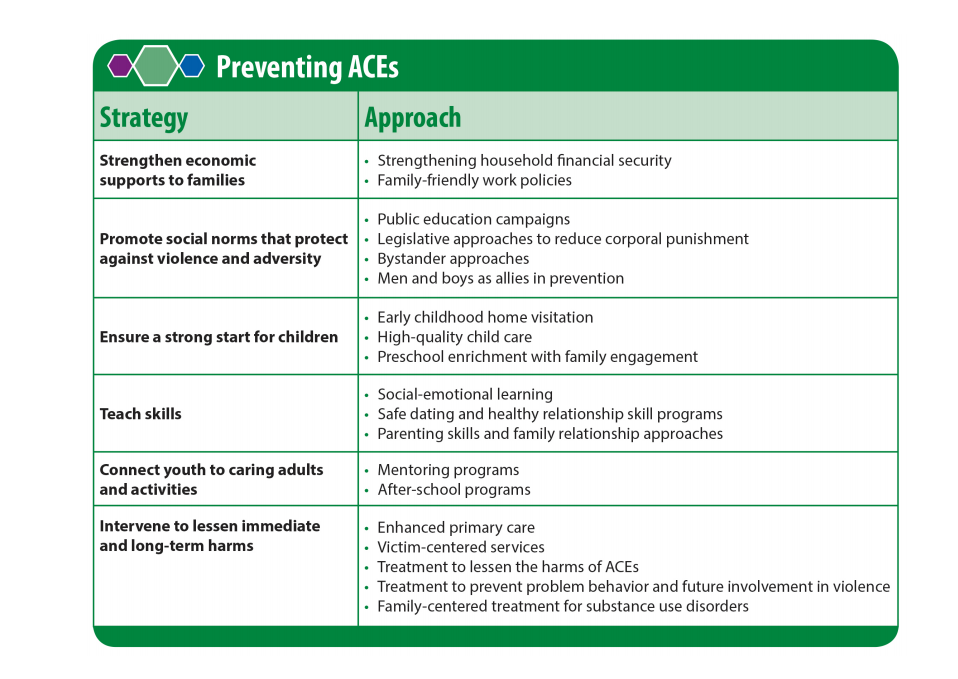
A critical strategy for primary prevention of ACEs and toxic stress in the public health setting begins with working upstream on the structural determinates of health to prevent child adversity from happening in the first place.
Daily Conditions
This means identifying and addressing the root causes, such as poverty, racism and discrimination, and distressed neighborhoods with underinvestment, issue that Latinos are disproportionately burdened by.
“Primary prevention interventions address the fundamental root causes of health status, such as housing security, economic supports, community development funds, living wage policies, family-friendly business policies, access to education, and employment opportunities,” Burke Harris’ roadmap states.
Interventions include:
- Expanding the reach and coverage of federal and state support mechanisms, such as Earned Income and Child Tax Credits, Supplemental Nutrition Assistance Program (SNAP), and housing subsidies
- Expanding the reach and coverage of opportunities like job skills, educational supports, and financial/economic literacy training
- Expanding paid family leave and paid sick leave laws
- Providing quality care and education early in life
- Reducing corporal punishment
- Providing access to high-quality mental and physical healthcare
- Teaching social-emotional learning, healthy relationship, and parenting skills
- Providing trauma-informed training for all child- and family-serving sectors
- Providing mentoring and after-school programs
- Promoting men and boys as allies in prevention
However, the “political will” to implement pro-child, pro-family policies and budgets is influenced by social norms about the status of children and the loci of responsibility for their well-being, according to Burke Harris’ roadmap.
This is problematic because the dominant public narrative about ACEs and childhood trauma has been characterized by an individual focus on “bad” parents, rather than a community focus on inadequate living conditions.
This is where public education comes in.
Public Education
The public health sector plays an important role in raising awareness about health issues and reframing those health issues in the broader context of social, economic, and environmental conditions.
For example, to counter individual-focused narratives, the FrameWorks Institute has created evidence-based tools to help increase public support for prevention and intervention policies that reduce child abuse and neglect.
“The future prosperity of our community/state/nation depends on our ability to foster the health and well-being of the next generation,” according to talking points from FrameWorks Institute. “Innovative states and communities have been able to design high-quality programs to reduce and prevent child abuse and neglect. These programs have created significant long-term improvements for children, and are the kind of innovations we need.”
The goal of this type of messaging is to unite people around shared values and a shared responsibility.
“Public health messaging and public education campaigns can be utilized to enhance public knowledge about ACEs, toxic stress, and their health impacts, and to bolster acquisition of concrete interventions and skills individuals can learn to regulate their stress responses, including improving sleep, nutrition, exercise, healthy relationships, access to nature, mindfulness practices, and when needed, mental healthcare, to build resilience,” Burke Harris’ roadmap states.
Public education campaigns can also promote social norms that protect against violence and adversity.
Primary prevention strategies must also work to improve public health care.
Secondary Prevention Strategies in Public Health
Secondary prevention, also known as early detection, aims to reduce the impact of ACEs that have already occurred before the development of toxic stress and associated health conditions.
This involves screening to identify risk factors and intervene as soon as possible. This is key to maintaining a tolerable stress response and halting or slowing the development of the toxic stress response.
Screening
Similar to screening children for lead exposure, screening children for toxic stress enables early detection and early intervention to prevent further adversity.
“Once ACEs and other risk factors of toxic stress occur, early detection, and early, evidence-based interventions are imperative to prevent toxic stress physiology from manifesting,” Burke Harris’ roadmap states.
However, there are no nationally agreed-upon biomarkers, tests, or diagnostic criteria for toxic stress.
While some potential biomarkers have been proposed, such as markers of inflammation, stress, altered metabolism, cellular aging, and epigenetic regulation, more research is needed to validate and translate biomarkers for use in clinical diagnosis and treatment.
Currently in California, healthcare providers use the Pediatric ACEs and Related Life-events Screener (PEARLS) test to assess children for the 10 original categories of ACEs—as well as seven additional categories of trauma.
Developed by the Bay Area Research Consortium on Toxic Stress and Health, diagnostic criteria for characterizing patient’s risk of manifesting a toxic stress response based on the 10 original ACE categories includes:
- A score of 0 indicates low risk, a score of 1-3 without associated health conditions indicates intermediate risk.
- A score of 1-3 with associated health conditions indicates high risk.
- A score of 4+ with or without associated health conditions indicates high risk.
More research can help “identify clinically useful biomarkers to diagnose and follow risk of toxic stress longitudinally, as well as more specific therapeutic targets,” Burke Harris’ roadmap states.
Data Collection
In the meantime, tracking population-level indicators of exposure to ACEs and impacts of toxic stress is important for the public health sector.
For example, in 2008, California became the first state to include questions about ACEs in the state’s Behavioral Risk Factor Surveillance System (BRFSS). The state currently collects information on eight out of the 10 ACEs.
“However, because the BRFSS ACE module is based on adults’ recollections of their childhoods, it is a lagging indicator of ACE exposure that doesn’t provide direct information about the current status of ACEs in California’s children,” Burke Harris’ roadmap states.
Learn more about other states that have done ACEs surveys from the ACEs Connections blog and interactive map.
The National Survey of Children’s Health and Maternal Infant Health Assessment survey are additional sources to monitor child adversity.
However, more community-level data are needed.
To achieve this, it is important for the public health sector to draw from solutions created to address other health conditions, like exposure to air pollution.
For example, to help decision-makers in California identify communities with exposure to air pollution, the California Environmental Protection Agency developed a mapping tool that uses 20 statewide indicators of pollution burden and population characteristics.
 “The tool includes data on air quality, drinking water quality, the presence of contaminated sites, and public health conditions such as low infant birth weight rates and asthma rates, as well as socioeconomic information such as poverty, educational attainment, and linguistic isolation,” Burke Harris’ roadmap states.
“The tool includes data on air quality, drinking water quality, the presence of contaminated sites, and public health conditions such as low infant birth weight rates and asthma rates, as well as socioeconomic information such as poverty, educational attainment, and linguistic isolation,” Burke Harris’ roadmap states.
This tool has been used to explore the relationship between vulnerable populations and the cumulative burden of multiple sources of pollution.
They found that more Latinx and Black individuals live in high pollution communities than other groups, who live in communities with lower levels of pollution.
A mapping tool like this could be developed to help public health professionals identify communities facing the cumulative burden of multiple risks factors for ACEs and toxic stress.
A more robust state and local data infrastructure is needed to move from population-level data to actionable community and clinical data.
Addressing Community Trauma
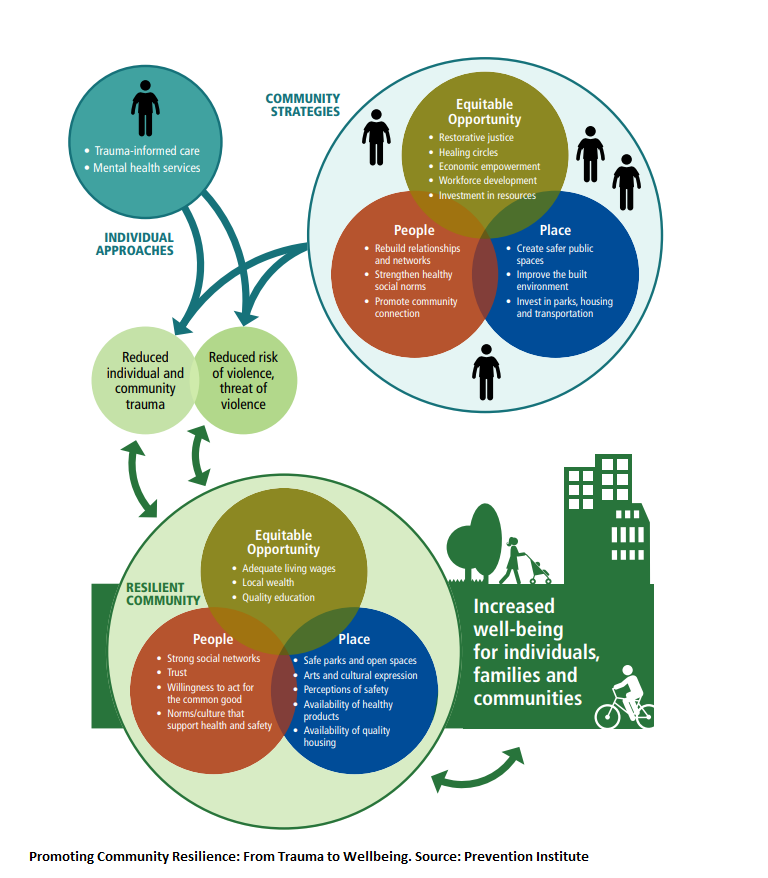
The impacts of ACEs extend beyond individuals and manifest at the community level.
“Community trauma is not just the aggregate of individuals in a neighborhood who have experienced trauma,” according to a report from the Prevention Institute.
When a community is traumatized, several inter-related components are undermined and damaged, so they begin to perpetuate the problems rather than protect the community.
“The result is both high levels of trauma across the population and a break-down of social networks, social relationships and positive social norms across the community—all of which could otherwise be protective against violence,” according to Prevention Institute.
Prevention Institute developed a framework to analyze community trauma and develop comprehensive strategies to address it.
Community-level strategies to address community trauma include:
- Revitalize damaged or broken social networks and infrastructure of social support
- Strengthen and elevate social norms that promote or encourage healthy behaviors, community connection and community-oriented positive social norms
- Provide a voice and element of power for community folks around shifting and changing environmental and structural factors
- Promote and restore a connection to and sense of cultural identity, which has been shown to have a positive impact on mental health outcomes
- Create safer public spaces through improvements in the built environment through addressing parks, housing quality, and transportation
- Institute restorative justice programs that shift the norms around conflict resolution and healing circles to, among other outcomes, support people to stay on paths to pursue educational and economic opportunities
- Foster economic and workforce development strategies that improve the employment skills, capacity and readiness of community members and link them to job opportunities with a living wage
- Increase community wealth and resources to reduce dislocation and gentrification
“Too many communities are plagued by trauma from experiencing adverse community conditions, including interpersonal violence and structural violence,” according to the Prevention Institute.
Tertiary Prevention Strategies in Public Health
Tertiary prevention, also known as early intervention or treatment, includes efforts that target individuals who have already developed a disease or social outcome.
“Strategies to address childhood trauma and adversity include efforts to help people regulate toxic stress physiology, a root cause of longer-term, often complex health consequences, in order to improve their ability to function, quality of life, and life expectancy,” Burke Harris’ roadmap states.
To support individuals who are assessed to be at intermediate or high risk for toxic stress, the public health sector can develop and support interventions and programs to address homelessness, teen pregnancy, criminal justice involvement, mental and behavioral health concerns, and other health and social conditions associated with ACEs and toxic stress.
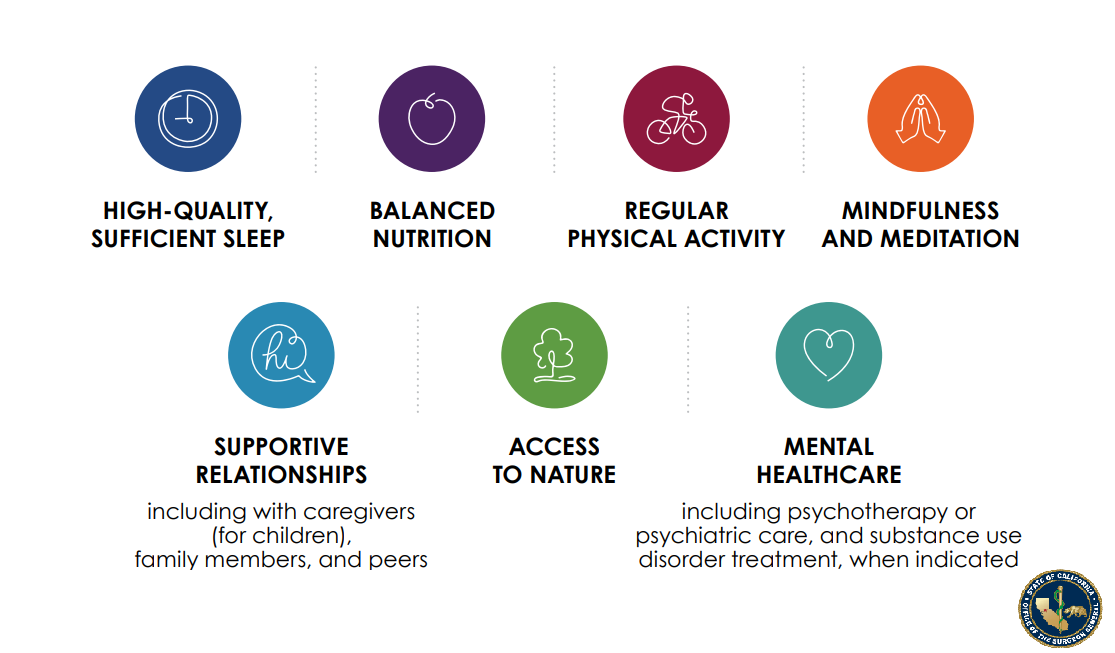
Similar to the healthcare sector, the public health sector should incorporate strategies to mitigate the toxic stress response, including social supports, regular exercise, mindfulness interventions, sleep hygiene, nutrition, and mental or behavioral health interventions.
Public health practitioners can also convene stakeholders to align multi-level, multi-faceted approaches; promote cross-sector collaboration and community engagement; and improve efficiency in implementing evidence-based interventions and policies.
Data monitoring systems, similar to the National Program of Cancer Registries, can aid in the collection and analysis of data on ACEs and toxic stress risk factors, incidence, and mortality.
These findings can then guide program monitoring, evaluation, and research.
“The use of population-level data collection and analysis to inform evidence-based screening, intervention, and evaluation of outcomes around ACEs, toxic stress, and AAHCs is also crucial,” Burke Harris’ roadmap states.
What You Can Do to Address Toxic Stress
Share our Salud America! team’s 11-part exploration into the important recommendations in Dr. Nadine Burke Harris’ roadmap to address ACEs and toxic stress:
- Toxic Stress and its Lifelong Health Consequences. Toxic stress is a public health crisis that has lifelong impacts on physical, mental, and behavioral health.
- We Need to Recognize Toxic Stress as a Health Condition with Clinical Implications. Health experts are pushing to elevate toxic stress and developmental trauma on national research and policy agendas.
- Cut Toxic Stress with 3 Types of Public Health Prevention Interventions. Preventing toxic stress requires a three-level public health intervention approach.
- How to Use Healthcare Strategies to Address Toxic Stress. In clinics, hospitals, and other healthcare settings, workers can provide universal trauma-informed care and more.
- Using Public Health Strategies to Address Toxic Stress. When it comes to ACEs and resulting toxic stress, the public health sector can play a critical role by strengthening economic support, positive family relationships, and social services. (current article)
- How to Use Social Service Strategies to Address Toxic Stress. We need trauma-informed training for social workers, as well as family-friendly workplaces and home visits.
- Toxic Stress in Early Childhood and How to Prevent It. Early childhood is a key time for preventing ACEs and toxic stress.
- Toxic Stress in Justice and How to Address It. Encounters with police are “intrinsically stressful and potentially traumatic,” especially for youth of color.
- Toxic Stress in Education and How to Address It. ACEs and toxic stress can hinder a person’s learning and school success.
- California’s Epic Response to Toxic Stress and ACEs. California, already leading the nation in addressing ACEs, is making inroads to address toxic stress.
- 5 Upstream Ways You Can Take Action to Address Toxic Stress. Here are ways you can take action to address toxic stress.
Read the public health sector brief.
Share this with friends, colleagues and public health professionals.
Urge them and local leaders to raise awareness about the impacts of ACEs and toxic stress through a coordinated public education campaign.
Push for a robust toxic stress data collection and research agenda.
“A collaborative ‘collective impact’ approach can mobilize efforts around the shared goal of reducing ACEs and toxic stress in half within a generation and recognizes the power of aligning cross-sector agency actors and community partners in mutually reinforcing policy, systems, and programmatic change activities,” Burke Harris’ roadmap states.
By The Numbers
142
Percent
Expected rise in Latino cancer cases in coming years



