
Share On Social!
To reduce the impact of a disease like diabetes, public health leaders usually apply a three-part preventive approach of prevention, early detection, and early intervention.
But this preventive approach hasn’t been applied to toxic stress.
Toxic stress is the body’s response to prolonged trauma─like abuse or discrimination─with no support. It can harm lifelong mental, physical, and behavioral health, especially for Latinos and others of color.
Amid COVID-19, civil unrest, and an economic crisis, we need a public health prevention approach to address toxic stress now more than ever.
A new roadmap can help.
Dr. Nadine Burke Harris’ Roadmap for Resilience: The California Surgeon General’s Report on Adverse Childhood Experiences, Toxic Stress, and Health proposes a three-part public health prevention approach to cut toxic stress in half within one generation.
Salud America! is exploring this as part of its 11-part series on toxic stress.
Why Is Toxic Stress a Big Deal for Lifelong Health─Just Like Diabetes?
Before we get to toxic stress, we have a question.
Do you think too much sugar is bad for you?
Our pancreas releases insulin to help our bodies deal with sugar. But some people don’t produce enough insulin or have become resistant. This is known as diabetes. And it can damage nerves, cause kidney failure, and lead to vision, liver, heart, and other problems.
To address diabetes, public health leaders have long applied the three-part intervention approach of prevention, early detection, and early intervention.
Toxic stress warrants a similar approach.
Just as some people struggle with diabetes because their bodies can’t properly deal with sugar, some suffer toxic stress because their bodies can’t deal properly with repeated trauma with no support.
Our adrenal gland releases adrenaline and cortisol to help our bodies deal with stress. Long-term adversity and trauma in childhood─from neglect and abuse to poverty and exposure to violence─can produce too much adrenaline and cortisol. This can elevate blood pressure and blood sugar, impair brain development and immune system function, disrupt neural connections, change how genes are read, and increase inflammation.
Toxic stress, in turn, can lead to lifelong physical, mental, and behavioral health problems, from heart disease to anxiety and depression to problems with attention and impulse control.
And the more trauma, the more toxic stress response, the more health problems.
For example, Latino kids exposed to many traumas are at increased risk for obesity, anxiety, withdrawal, aggression, substance abuse, and lower academic skills, according to a Salud America! research review.
Adults are not exempt, either.
Burdens from COVID-19, racism, and discrimination are some of the severe, intense, or prolonged stressors that cause toxic stress response in adults.
You can read more about toxic stress here.
So how can we address toxic stress like public health leaders do for diabetes?
How Can We Use Prevention Strategies, Public Health’s Primary Tool for Prevention, to Address Toxic Stress?
Burke Harris’ new roadmap provides prevention (primary), early detection (secondary), and early intervention (tertiary) strategies so policymakers, scientists, healthcare providers, educators, and advocates can prevent toxic stress and address trauma.
First up is primary prevention.
This includes efforts that target healthy individuals and aim to prevent harmful exposures and behaviors from ever occurring.
Primary prevention aims to change structural and systemic conditions to prevent unhealthy behaviors and risk factors, and increase healthy behaviors and protective factors.
 Similar to addressing systemic inequities to improve healthy equity, primary prevention efforts require upstream investment and policy change to change the environment in which people live, learn, work, and play so that everyone has a fair chance to achieve health.
Similar to addressing systemic inequities to improve healthy equity, primary prevention efforts require upstream investment and policy change to change the environment in which people live, learn, work, and play so that everyone has a fair chance to achieve health.
Here are some examples of primary prevention strategies for diabetes, COVID-19, and toxic stress:
- For diabetes: Primary prevention strategies are designed to prevent and reduce sedentary behavior and unhealthy diets. These include efforts to make streets safer and communities more walkable; increase access to parks and healthy food; improve meals and increase time for physical activity in early child care and K-12 education; and educate the public about the harms of sugary drinks.
- For COVID-19: Primary prevention strategies are designed to prevent and reduce the transmission of an infectious disease. These include polices requiring masks and limiting occupancy in public places, paid sick leave and family medical leave policies, efforts to encourage working from home, vaccinations, and campaigns to educate the public about infection prevention measures.
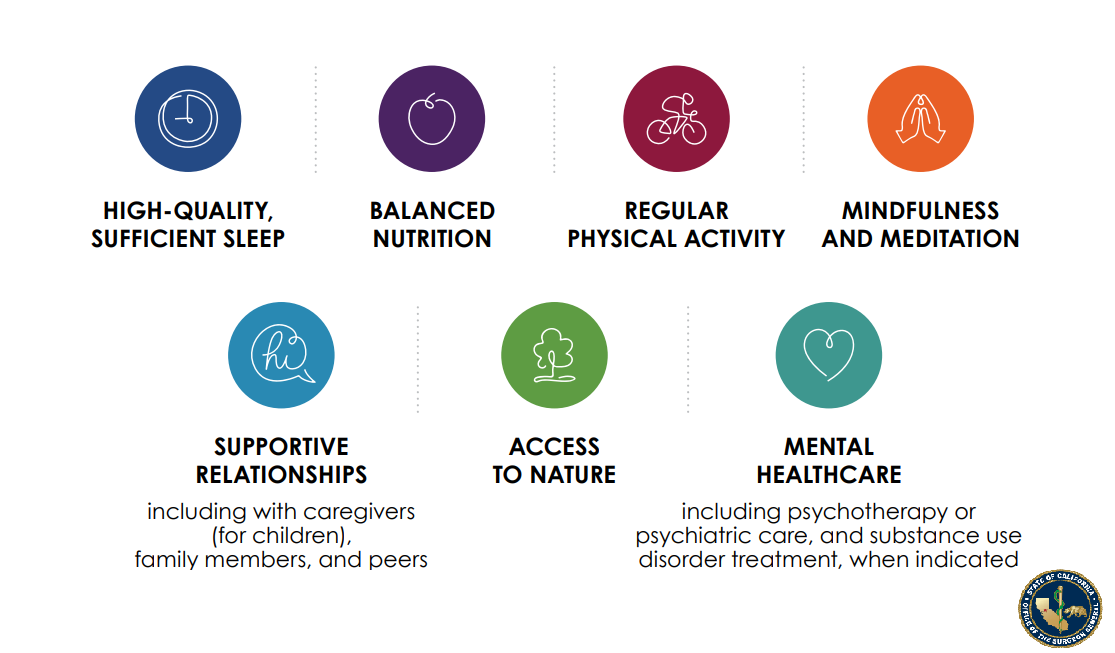
- For Adverse Childhood Experiences (ACEs) and toxic stress: Primary prevention strategies are designed to prevent and reduce the likelihood of severe, intense, or prolonged stress, trauma, or adversity from ever occurring. These include efforts to reduce poverty and food insecurity, improve early care and education opportunities, enhance parenting attachment and family bonds, increase access to mental and physical healthcare, educate the public about the biology of toxic stress, and increase access to opportunities for stress-buffering activities such as parks, mindfulness activities, physical activity, and sleep.
“In 2020, multiple simultaneous public health emergencies have laid bare the substantial structural and systemic forces that imperil health and well-being,” Burke Harris’ roadmap states. “It is clear that vulnerable and systematically overlooked communities bear the brunt of each new crisis, and that these communities deserve a much more effective set of buffering systems and supports.”
Additional primary prevention strategies to address toxic stress include:
- Healthcare: provide universal trauma-informed care, patient education, anticipatory guidance, and important linkages to cross-sector partners, as well as advocate for trauma-informed systems and effective referral networks.
- Public Health: Strengthen economic supports for families and promote safe and stable supportive housing.
- Social Services: increase family-friendly work environments (e.g., paid family leave, on-site child care) and improve neighborhood safety and play areas for children.
- Early Childhood Supports: preventing adverse experiences and strengthening buffering influences, typically by creating policies and programs that promote safe, stable, nurturing early relationships and environments.
- Education: Trauma-informed training and principles for all staff and promoting of a safe, calm, supportive, predictable, and nurturing environment and a positive school climate.
- Justice: Limit zero-tolerance policies, increase police accountability, and reduce the school-to-prison pipeline.
“Based on a comprehensive public health framework, primary prevention strategies are rooted in ensuring broad public awareness and supported by effective upstream policy and systems changes, such as assuring social, educational, and economic opportunities for all, support of social safety net programs, and proactive actions that promote equity, including anti-racist frameworks,” Burke Harris’ roadmap states.
In January, 20201, the International Transformational Resilience Coalition (ITRC), released the ITRC Mental Wellness and Resilience Policy calling for a public health prevention approach to preventing and healing toxic stress generated by the climate emergency.
“The public is unprepared for the psychological and emotional toll generated by accelerating climate change generated disasters and pileups of toxic stresses,” the policy guide states.
The ITRC policy calls on Congress to enact and fund the Mental Wellness and Resilience Act (MWRA) to make the prevention of mental health and psychosocial problems a national priority and calls on the establishment of an Office of Mental Wellness and Resilience in the Department of Health and Human Services.
The ITRC policy also calls for the formation of Resilience Coordinating Councils in every community or region nationwide. These councils should focus on:
- teaching trauma-informed mental wellness and resilience information and skills to all adults and youth;
- repairing and building individual, family, and community strengths;
- establishing and connecting quality social support networks across economic and geographic boundaries;
- empowering residents to take responsibility for building resilience at the neighborhood level; and
- engaging local organizations of all types in the development of social norms that promote safe, healthy, just, and equitable responses to adversities and enable people to find new constructive sources of meaning, purpose, and hope.
“The ITRC policy calls for the establishment of community-based culturally-grounded initiatives nationwide to build and sustain mental wellness and resilience within entire populations for the combo of climate disasters, emergencies, and pileups of toxic stresses, as well as many other adversities,” the ITRC report states.
How Can We Use Early Detection Strategies, Public Health’s Secondary Tool for Prevention, to Address Toxic Stress?
Early detection, also known as secondary prevention, involves screening to identify risk factors and/or diseases in the earliest stages, before the onset of signs and symptoms.
The goal is to target interventions to those who need them most early, when interventions are likely to be more effective and less expensive. Read more about the financial costs of ACEs and toxic stress here.
Breast cancer screenings, for example, increased early-stage disease detection and decreased the incidence of late-stage, averting roughly 375,900 deaths between 1989 and 2017.
Screening, however, requires evidence-based biomarkers to test and diagnostic criteria to determine to what is or isn’t normal function.
Here are some examples of secondary prevention strategies for diabetes, COVID-19, and toxic stress:

For diabetes.
- Secondary prevention strategies include hemoglobin A1C testing. The A1C test measures percent of red blood cells that have sugar-coated hemoglobin—the biomarker—in your blood to determine blood sugar levels over the past three months. The diagnostic criteria include the following: an A1C level below 5.7% is normal, an A1C level of 5.7% to 6.4% indicates prediabetes, and an A1C level of 6.5% or above indicates diabetes.
- A1C is one tool for managing diabetes but does not replace regular blood sugar testing because blood sugar may go up and down throughout the day and night. The diagnostic criteria for regular blood sugar monitoring recommends a normal range if results are 80 to 130 mg/dL (milligrams of glucose per deciliter of blood) before meals and below 180 after meals.
- Secondary prevention strategies also include educating individuals identified with high blood sugar about healthy eating and physical activity to prevent disease onset.
For COVID-19.
- Secondary prevention strategies include molecular or antigen tests. The molecular test measures genetic material that comes from SARS-CoV-2—the biomarker—in the nose, throat, or other areas in the respiratory tract to determine if genetic material is present. Diagnostic criteria are positive detection of genetic material means an individual currently has an active infection. However, failure to detect genetic material does not mean an individual does not have an active infection. Similarly, antigen tests measure proteins that come from SARS-CoV-2—the biomarker—and positive detection meets the diagnostic criteria for an active infection.
- Secondary prevention strategies also include case investigation and contact tracing where public health workers contact infected and exposed individuals to encourage them to isolate and monitor symptoms.
For ACEs and toxic stress.
- Secondary prevention strategies include ACEs screenings to identify individuals with risk factors for having a toxic stress response.
- The Pediatric ACEs and Related Life-events Screener(PEARLS) test is used by healthcare providers in California to assess children for the 10 original categories of ACEs—as well as seven additional categories of trauma. Developed by the Bay Area Research Consortium on Toxic Stress and Health (BARC), diagnostic criteria for characterizing patient’s risk of manifesting a toxic stress response based on the 10 original ACE categories includes: a score of 0 indicates low risk, a score of 1-3 without associated health conditions indicates intermediate risk, a score of 1-3 with associated health conditions indicates high risk, and a score of 4+ with or without associated health conditions indicates high risk.
- Unfortunately, there are no nationally agreed-upon biomarkers, tests, or diagnostic criteria for toxic stress. While some potential biomarkers have been proposed, such as markers of inflammation, stress, altered metabolism, cellular aging, and epigenetic regulation, more research is needed to validate and translate biomarkers for use in clinical diagnosis and treatment.
- Secondary prevention strategies also include applying principles of trauma-informed care, providing referrals to patient resources or interventions, and providing patient education on toxic stress and strategies to regulate the stress response including, supportive relationships, regular exercise, access to nature, sufficient and high-quality sleep, balanced nutrition, mindfulness practices, and mental and behavioral healthcare.
“Once ACEs and other risk factors of toxic stress occur, early detection, and early, evidence-based interventions are imperative to prevent toxic stress physiology from manifesting,” Burke Harris’ roadmap states.
In addition to identifying patients at high risk of developing negative health outcomes, early detection provides an opportunity to apply targeted interventions to prevent further exposures, strengthen existing protective factors, provide buffering care, and ultimately prevent toxic stress physiology and downstream consequences, such as earlier-onset, more severe health conditions or toxic stress-related social consequences.
“More research is needed to precisely identify clinically useful biomarkers to diagnose and follow risk of toxic stress longitudinally, as well as more specific therapeutic targets,” Burke Harris’ roadmap states.
Additional secondary prevention strategies to address toxic stress include:
- Healthcare: Facilitate early detection through routine screening and apply buffering interventions.
- Public Health: Surveillance of population-level indicators of exposure to ACEs and impacts of toxic stress, with policy-oriented application of this data.
- Social Services: Home visiting programs that provide support and assistance to families at risk of abuse or neglect.
- Early Childhood Supports: home visitation programs, connection to economic and other parenting supports, and educational opportunities for parents and early childhood professionals about ACEs and toxic stress, long-term health and developmental impacts, and strategies relating to caregiver self-care, and positive, buffering interventions focused on preventing the transmission of adversity.
- Education: Training on ACEs and toxic stress to include skills to identify early signs and symptoms and restorative discipline practices to avoid retraumatization.
- Justice: Training correctional staff in trauma-informed justice practices.
“California has allocated $143.1 million over two fiscal years (2019/20 and 2020/21) to support training and reimbursement for provider screening and response for ACEs and toxic stress among eligible children and adults receiving Medi-Cal,” according to a brief from the Office of the California Surgeon General.
How Can We Use Early Intervention Strategies, Public Health’s Tertiary Tool for Prevention, to Address Toxic Stress?
Early intervention or treatment, also known as tertiary prevention, includes efforts that target individuals who have already developed a disease or social outcome.
The goal is to lessen the severity, progression, or complications associated with the disease or social outcome.
Here are some examples of tertiary prevention strategies for diabetes, COVID-19, and toxic stress:
- For diabetes: Tertiary prevention strategies include diabetes medication, insulin therapy, medical nutrition and physical activity therapy, and blood sugar monitoring.
- For COVID-19: Tertiary prevention strategies include antiviral medication, steroid medication, oxygen therapy, convalescent plasma therapy, and mechanical ventilation.
- For ACEs and toxic stress: Tertiary prevention strategies include efforts to regulate the stress response system. These include enhancing supportive relationships, regular exercise, more access to nature, sufficient and high-quality sleep, balanced nutrition, mindfulness practices, and mental and behavioral healthcare. Unfortunately, due to limited research, there are no precision medicine treatments for toxic stress.
Because toxic stress is intergenerational, wherein parental biology or behavior affects the development and health of their children, secondary or tertiary prevention—or detection and treatment of toxic stress—in one generation is primary prevention for the next. It also prevents adversity and other risk factors for the next generation.
Additional tertiary prevention strategies to address toxic stress include:
- Healthcare: implement tools and interventions that target the underlying biological mechanisms of toxic stress to reduce the impact of the toxic stress response and improve neuroendocrine-immune-metabolic functioning.
- Public Health: Facilitate treatment of toxic stress among adults to prevent intergenerational transmission.
- Social Services: Intensive family preservation services, with trained mental health counselors that are available to families for intensive bursts.
- Early Childhood Supports: engage trained mental health counselors for intensive family preservation services, coordinate parent support groups to share best practices on positive parenting behaviors and attitudes, recruit parent mentors to serve as role models to families in crisis, and deploy mental health services to bolster effective communication and family cohesion.
- Education: Close coordination between school and healthcare personnel, such as in implementing individualized education programs (IEPs) and referrals to needed healthcare services, as well as school-based health services targeting toxic stress, such as mental health and mindfulness interventions.
- Justice: Provide preventative and treatment-oriented physical and mental healthcare for justice-involved or incarcerated individuals.
“California is advancing tertiary prevention of ACEs and toxic stress by providing up to $9 million through the California Initiative to Advance Precision Medicine to competitively fund three to five projects to demonstrate precision medicine approaches to addressing ACEs and toxic stress through research partnerships between academic centers and community or public health organizations,” according to a brief from the Office of the California Surgeon General.
Addressing toxic stress needs to be a cross-sector effort with sustained collaborations between the healthcare, public health, social services, education, justice, and other allied sectors.
What You Can Do to Address Toxic Stress
Share our Salud America! team’s 11-part exploration into the important recommendations in Dr. Nadine Burke Harris’ roadmap to address ACEs and toxic stress:
- Toxic Stress and its Lifelong Health Consequences. Toxic stress is a public health crisis that has lifelong impacts on physical, mental, and behavioral health.
- We Need to Recognize Toxic Stress as a Health Condition with Clinical Implications. Health experts are pushing to elevate toxic stress and developmental trauma on national research and policy agendas.
- Cut Toxic Stress with 3 Types of Public Health Prevention Interventions. Preventing toxic stress requires a three-level public health intervention approach (current article)
- How to Use Healthcare Strategies to Address Toxic Stress. In clinics, hospitals, and other healthcare settings, workers can provide universal trauma-informed care and more.
- Using Public Health Strategies to Address Toxic Stress. When it comes to ACEs and resulting toxic stress, the public health sector can play a critical role by strengthening economic support, positive family relationships, and social services.
- How to Use Social Service Strategies to Address Toxic Stress. We need trauma-informed training for social workers, as well as family-friendly workplaces and home visits.
- Toxic Stress in Early Childhood and How to Prevent It. Early childhood is a key time for preventing ACEs and toxic stress.
- Toxic Stress in Justice and How to Address It. Encounters with police are “intrinsically stressful and potentially traumatic,” especially for youth of color.
- Toxic Stress in Education and How to Address It. ACEs and toxic stress can hinder a person’s learning and school success.
- California’s Epic Response to Toxic Stress and ACEs. California, already leading the nation in addressing ACEs, is making inroads to address toxic stress.
- 5 Upstream Ways You Can Take Action to Address Toxic Stress. Here are ways you can take action to address toxic stress.
Share this with friends and colleagues to raise awareness about the impacts of ACEs and toxic stress through a coordinated public education campaign.
Urge local leaders to recognize and respond to toxic stress using the three-part public health approach to prevention.
“To truly transform the negative outcomes associated with ACEs, California, as well as other states and nations, must act intentionally and inclusively to address the structural factors that result in disparities in health, social, and economic outcomes and opportunities,” Burke Harris’ roadmap states.
By The Numbers
142
Percent
Expected rise in Latino cancer cases in coming years



